Case Report - (2021) Volume 8, Issue 6
A case report on management of recurrent pediatric fistula in ano with an udumber ksheersutra varti
Kiran Khandare1*, Aditya Trivedi1, Monika Meshram1 and Pradnya Ghormode2Abstract
Fistula-in-ano and Perianal abscess are common findings in infants and children. The perianal abscess is usually a manifestation of a fistula-in-ano. Although surgical treatment is an extensively standard remedy for fistula-in-ano, it was recently advised that fistula-in-ano in toddlers is a time-confined disease and fistulotomy or fistulectomy must be avoided. However, it should be noted that conservative treatment of fistula leads to prolonged hospital stay, prolonged antibiotic use and additional pain. Although recurrence of a perianal abscess or fistula abscess after treatment is possible, there should be undue evidence of suspected Crohn’s disease in older young people who wish to relapse. We aimed to present the optimal management of fistula-in-ano in order to reduce or even eliminate the risk of recurrence. It was also discovered that udambara ksheera heals vital recurrent anal fistulas by acting on its shodhan (wound cleaning) and ropan (wound healing) properties. So present case study of reccurrent fistula in ano in pediatric patient was carried out in outpatient department of Shalya Tantra at Mahatma Gandhi Ayurved College, Hospital and Research Centre, Salod (Hirapur) under Datta Meghe Institute of Medical Sciences, which was successfully treated.
Keywords
Udambara ksheera sutra, recurrent anal fistula, ropan, shodhan
Introduction
According to Acharya Sushruta, Bhagandar was considered as one of the Ashtamahagad, this demonstrates the seriousness of the disease. It appears as Pidika at first, then becomes Pakwa to form Bhagandar in Bhaga , Guda, and Basti Pradesh, it causes Daran [1]. it can be co releated with fistula in ano in morden science. Anal fistulas are relatively common conditions in the pediatric population, especially in infancy.
Inflammation of the glands located in abnormally deep Morganini’s crypts is the cause of development of perianal abscesses and fistulas [2]. Inflammation is initiated in the crypts and spreads to the surrounding tissues, leading to inflammation and formation of an abscess in that area. In most patients, perianal abscess is a symptom and consequence of anal fistula running from the crypt on the top of the anal canal to the skin. The largest group of patients comprised male infants without other chronic conditions. There are disagreements among numerous researches approximately the charges of recurrence of anal fistula in ano. Some researchers [3] encouraged lively probing for underlying fistula in ano in all children undergoing surgery. It is found in present day surgical technological know-how maximum common surgery followed with inside the treatment of fistula in ano are fistulectomy, fistulotomy, flap advancement, LIFT, glue, and seton. These surgical control includes numerous complications like frequent harm to the anal sphincters muscles, faecal soiling, rectal prolapse, anal stenosis, not on time wound healing, or even after entire excision of tract there are possibilities of recurrence [4]. In earlier studies it is reported that the latex expressed from certain plants can be very well used to prepare the ksheer sutra which is having very good effect in fistula-in ano [5] by reducing the pain with the usual advantages of kshara sutra, Lack of consensus in the treatment of this disease makes choosing treatment difficult and in infants it is very difficult to manage the pain, inflammation, infection therefore in this present study udumber ksheersutra varti is used in this case of recurrence fistula in ano.
Case Report
A six month old male infant was brought to Shalyatantra Out-patient Department (OPD) with complaints of pus and sometimes bloody discharge from the boil present at perianal region. His mother narrated complaints that baby cries very loudly for a long period of time after defecation. After a day or two, boil disappeared without any treatment and again the same boil appeared with discharge. Mother got sentimental while giving history of previous operation of her four months baby for same complaints and she provided documents of previous operation done in a private hospital. As per the documentary evidence, at the age of 4 months before surgery high resolution USG local region shows-in perianal region at 3 o’clock position s/o small perianal abscess opening in anal canal by fistulous tract of length about 16.5 mm long running upwards, inwards and medially and opening in anal canal about 6.3 mm above the anal verge.
Other document provided shows that fistulectomy was done under general anaesthesia with satisfactory post operation recovery and specimen send for histopathology.
Histopathology report revels received multiple, irregular, very scant, white yellow tissue piece aggregating less than 0.2 × 0.2 cm. Section from soft tissue biopsy shows histopathological features consistent with fistula in ano and in view of clinical details.
On examination, vitals and systemic examination was normal. Local examination shows redness and boil with pus discharge oozing from external opening present in left gluteal region at 3 o’ clock position approximately 4–6 cm from anal verge. On palpation revealed tenderness and raised local temperature and induration is present communicating to anal canal and show fluctuation test negative. On digital examination with little finger, sphincter tone appears normal, there was no internal opening felt or active bleeding seen during examination. After clinical examination this case was diagnosed as recurrence case of fistula in ano after fistulectomy surgery.
Treatment Given
Mother of this infant is not willing for any surgical procedure therefore we planned for some parasurgical or conservative treatment in this case. Application of ksharsutra in the fistula tract is not possible without anaesthesia therefore the application of udumber ksheersutra varti was planned for the treatment of this recurred fistula. After completing all legal formalities and following protocol of hospital, written consent was taken from parent. The application of udumber ksheersutra varti is done after all aseptic precautions without anaesthesia as this is a simple parasurgical procedure mentioned in Ayurveda.
In lithotomy position a ksheersutravarti was inserted from the external opening of the fistula and dressing done with sterile dry gauze and then this varti was allowed to remain in the tract for at least 10 to 12 hours. After 12 hrs external opening was clean with antiseptic solution and left opened. Parents of patient were advised to visit hospital after the appearance of boil and then same procedure was carried out.
After six udumber ksheersutra varti procedures in a period of 27 days, patient recovered completely and there no sign of fistula was noted after the treatment. No other medicine was prescribed in this case except the regular mother breast feeding. Fistula tract was completely healed without any discharge (Fig 1 and 2), later the patient was followed up for a period of 6 months and no recurrence of symptoms was observed.
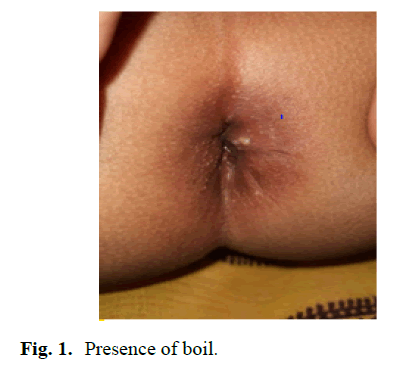
Figure 1: Presence of boil.
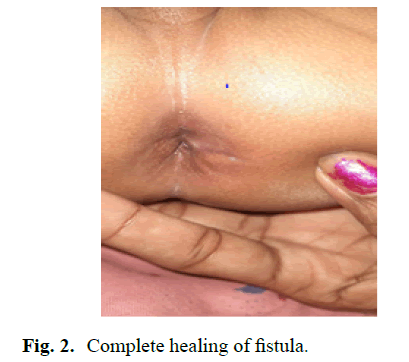
Figure 2: Complete healing of fistula.
Results and Discussion
The glands of hermann and desfosses, which are located within the thickness of the anal canal, open into the canal at the dentate line. Infection of these anal glands leads to the formation of abscesses and/ or fistulas. If these manifests as an abscess, emergency drainage of the infected cavity is required [6]. Anal sepsis in children ranges from perianal abscess to fistula. It is mainly determined in children under 2 years of age. Most are running conservatively. In contrast, anal sepsis in older children is clearly similar to that in adults, and is mainly treated with surgery. Fistulas can be treated with fistula incision or fistula resection, both of which are related to the reasonable possibility of fistula recurrence [7]. The plan of care proceeded with Udumber ksheer varti and sitz bath which helps in maintaining the hygiene of perineal and peri-anal area and reducing the inflammation, pain and relaxed the spasm of sphincter muscles [8]. Udumber ksheer has activities including wound healing, antidiabetic, antibacterial, anti-inflammatory, hepatoprotective, and antimicrobial activities [9]. Udumber ksheer is having shodhana and ropana properties. When applied topically, Shodan medicine can reduce pain, discharge and swelling of surrounding tissues [10]. These drugs initially act as cleansers, removing exfoliated and necrotic materials from the wound, and ultimately promote clean and clear healing. They reduce wound contamination by bactericidal action on drug-impregnated shodhana dressings, and provide a moist environment to supplement epithelial formation and prevent exfoliation, which is beneficial to inflamed wounds with resistant bacteria. After 3 sitting of application wound was found healthier and reduced the pain and discomfort [11]. Related studies from modern medicine were reviewed [12-17].
Conclusion
This case report is an attempt to show the effectiveness of udumber ksheersutra varti in management of recurrent fistula-in-ano in pediatric patient. The patient has been effectively treated without the need for any surgical intervention. The condition and progress of the patient have been properly documented photographically. Reduce pus, healthy granulation tissue and fully healed cavity. Udumber ksheer varti has the properties of Shodhana and Ropana, as well as an antibacterial effect that promotes blood vessel formation and cavity healing. Following the treatment there was no recurrence of abscess formation and no formation of fistula. So Udumber ksheersutra varti can be used in perianal abscess as local application and is very cost effective also.
References
- Sushrut Samhita, Ayurved tatva sandipika with hindivyakhya. Edition 2012; Sutrasthana 33/4.
- Shafer AD, McGlone TP, Flanagan RA. Abnormal crypts of morgagni: The cause of perianal abscess and fistula-in-ano. J Ped Surg. 1987; 22:203-4.
- Piazza DJ, Radhakrishnan J. Perianal abscess and fistula-in-ano in children. Dis Colon Rectum. 1990; 33:1014-1016.
- Williams N, O'Connell PR. Bailey & love's short practice of surgery. 2008; 1264.
- Acharya Vaidya JT, Acharya N. Chowkhambha surabharati prakashan. 2008.
- Pigot F. Treatment of anal fistula and abscess. J Visc Surg. 2015; 152:S23-9.
- Charalampopoulos A, Zavras N, Kapetanakis EI, et al. Surgical treatment of perianal abscess and fistula-in-ano in childhood, with emphasis in children older than 2 years. J Pediatr Surg. 2012; 47:2096-100.
- Ezer SS, Oğuzkurt P, Ince E, et al. Perianal abscess and fistula‐in‐ano in children: Aetiology, management and outcome. J Paediatr Child Health. 2010; 46:92-5.
- Kurapati VK, Nishteswar K. Management of ano-rectal disorders by kṣārasūtra: A clinical report. Anc sci life. 2014; 34:89-95.
- Ahmed F, Urooj A. Traditional uses, medicinal properties, and phytopharmacology of ficus racemosa: A review. Pharm Biol. 2010; 48:672-81.
- Chandravanshi S, Swer JK, Shailaja SV. A case study of perianal abscess in hyperglycemic patient. Int Ayurved Med J. 2017.
- Sankalp D, Joharapurkar SR, Abhay D. Double breasting repair of urethral fistula in a patient with perineal abscess secondary to a large urethral stone. Indian J Plast Surg. 2008; 41:226-8.
- Swarnkar M, Bagasrawala S, Shinde RK, et al. Sphincter-preserving therapy with topical 2% diltiazem for chronic anal fissure: Our experience. J Krishna Inst Med. 2015; 4:36-41.
- Diwedi AK, Khandare K. A rare case of anal condyloma in AIDS patient. Pan Afr Med J. 2020; 37.
- Khandare K, Ghormode P. Prolapsed rectal submucosal hematoma in pediatric case. Pan Afr Med J. 2020; 37.
- Mithra P, Khatib MN, Sinha AP, et al. Interventions for addressing anemia among children and adolescents: An overview of systematic reviews. Front Pediatr. 2021.
- Dangre G, Tankhiwale N, Mudey A. Antimicrobial resistance in neonatal septicaemia: A therapeutic challenge to pediatricians of rural India. Int J Infect Dis. 2012; 16:e412.
Author Info
Kiran Khandare1*, Aditya Trivedi1, Monika Meshram1 and Pradnya Ghormode22Department of Sharir Rachana, DMM Ayurved Mahavidyalaya, Yavatmal, Maharashtra, India
Received: 03-Dec-2021 Accepted: 17-Dec-2021 Published: 24-Dec-2021, DOI: 10.14534/j-pucr.2022.282
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
