Case Series - (2023) Volume 10, Issue 6
A complete epididymo-testicular non-union: Three case reports
Stijn van Sas*Abstract
Testicular-Epididymal Fusion Anomalies (TEFA) is rare developmental abnormalities affecting the male reproductive system. We present 3 cases of complete epididymo-testicular non-union, a severe form of TEFA, and discuss their clinical presentation, diagnostic workup, surgical and anatomopathological findings. This case report highlights the importance of early diagnosis and tailored surgical interventions based on testicular viability and mobility. Long-term follow-up will be necessary to evaluate testicular function and fertility potential.
Keywords
Epididymo-testicular, non-union, nubbin, testis, undescended
Introduction
Testicular-Epididymal Fusion Anomalies (TEFA) is unusual developmental abnormalities that affect the male reproductive system. These anomalies occur when the testis and epididymis fail to properly fuse during embryonic development [1]. This fusion process involves a well-organized series of molecular and morphogenic events, and any disruptions in this process can result in defects in these organs and their interconnections, potentially causing TEFA [1].
The impact of these defects can vary widely. Some may be inconsequential, while others can interfere with the formation and transportation of semen in adult males, causing fertility issues [2,3]. TEFA is often associated with cryptorchidism and is classified into different types based on the extent of disruption, including head, tail, and complete non-union [2].
In cases of complete epidimo-testicular non-union, the testis is positioned either within the inguinal canal or in the abdomen, while the vas deferens leads to scrotal nubbin tissue. A meta-analysis by Qin, et al. shows that TEFA affects approximately 26% of cryptorchid testes, with around 6% being complete non-fusion, resulting in impaired sperm transport [2].
Case Presentation
Case 1
A 3-year-old boy was referred to the urology clinic due to suspicion of a left-side hydrocoele. Following a clinical examination and ultrasound, a retractile left testis and a non-communicating hydrocoele were suspected. A conservative approach was chosen initially. 6 months later, a repeated scrotal ultrasound revealed a normal position and appearance of the right testis (13.6 × 8.1 mm) and epididymis, while on the left side intrascrotally only non-compressible fluid (14 × 5 mm). The left testis was located low para-iliacally above the inguinal canal, normal in appearance and size (12.8 × 7.1 mm). Based on these findings, the diagnosis of leftsided cryptorchidism with hydrocoele fluid, possibly with an open processus vaginalis, was made, and an orchidopexy on the left side was planned.
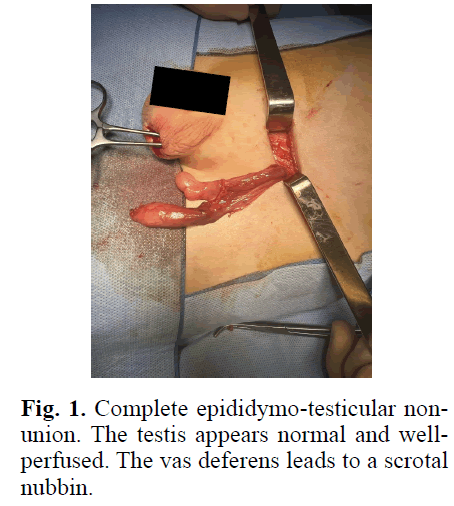
Intraoperatively, an epididymo-testicular non-union was identified, with the vas deferens leading to a scrotal nubbin. Despite this anomaly, the testis appeared normal and well-vascularized. The scrotal nubbin was ligated and removed. The testis was then brought into the scrotum and fixed in place.
The anatomical pathology report indicated that the scrotal nubbin comprised edematous fibroadipose tissue, with interposed muscle tissue and remnants of the epididymis. Additionally, some sections were suggestive of being from the vas deferens. Notably, no recognizable (atrophic) testis remnants were observed, confirming the diagnosis of complete epididymotesticular non-union (Figure 1).
Fig. 1. Complete epididymo-testicular nonunion. The testis appears normal and wellperfused. The vas deferens leads to a scrotal nubbin.
Case 2
A 9-year-old boy, presented to the urology clinic with a diagnosis of cryptorchidism. The ultrasound examination revealed normal position, size (19 × 7 × 15 mm) and appearance of the right testis, while the left testis was located intra-abdominally, anterior of the external iliac artery with a more elongated shape (19 × 4 × 9 mm). The scrotal wall appeared normal, without any hydrocele or varicocele.
The treatment plan involved a laparoscopic exploration with orchidopexy if the left testis was viable. Alternatively, orchidectomy was considered if the testis showed signs of involution.
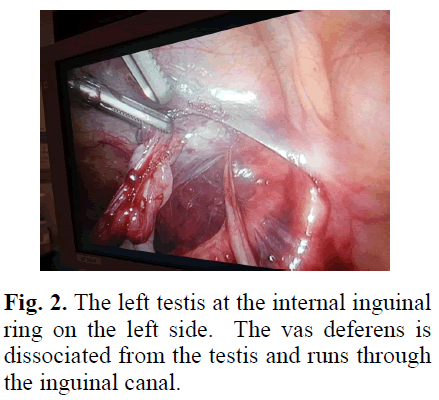
During the laparoscopic exploration, the testis was visualized at the internal inguinal ring. Dissection of the gubernaculum and ductus revealed that the vas deferens was dissociated from the testis and ran through the inguinal canal, likely toward an epididymal remnant. Due to insufficient vascular length, the testis could not be adequately mobilized. As a result, the ductus with the epididymal remnant was resected, followed by the excision of the testis (Figure 2).
Fig. 2. The left testis at the internal inguinal ring on the left side. The vas deferens is dissociated from the testis and runs through the inguinal canal.
Case 3
The A 15-year-old boy with pubertal characteristics Tanner stage IV, was referred to the urology department due to atrophic left testis. The patient has had this condition his entire life and experienced no discomfort.
Clinical examination revealed that the left testis was presumably fixed at the external annulus. A fluidcontaining structure was found in the left scrotum and the right testis was of normal size and aspect, normally descended with a dissociated epididymis. An initial scrotal ultrasound showed an atrophic appearance of the longtestis and a fluid collection in the left scrotum.
The conclusion was left-sided cryptorchidism with clinical suspicion of a free atrophic testis in the left groin. A more targeted scrotal ultrasound confirmed the normal position and aspect of the right testis, while the left testis was located distally in the inguinal canal and measured 44 × 9 × 20 mm, showing normal blood flow. The parenchyma appeared relatively hyposonant compared to the right testis, no suspicious inlying abnormalities were found.
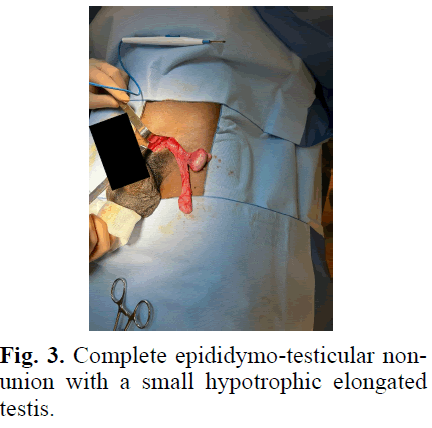
The preferential diagnosis was left-sided cryptorchidism, postpubertal hypotrophic testis. It was decided to perform an inguinal orchidectomy given increased risk of malignancy. During the procedure, epididymo-testicular non-union was observed with a small hypotrophic elongated testis.
Anatomical pathology report revealed a hypotrophic testis with numerous tubules lined by multilayered epithelium, exhibiting no clear spermatogenesis. The interstitial stroma appeared loose. A tissue section at the cut edge exhibited a tubular structure lined by multilayered epithelium, surrounded by fibrous tissue with several thick-walled vascular structures. Another tissue section at the loose cord displayed dilated glandular structures lined by multilayered, ciliated epithelium, along with a small fragment of rete with no abnormalities detected. Importantly, there were no indications of dysplasia or malignancy (Figure 3).
Fig. 3. Complete epididymo-testicular nonunion with a small hypotrophic elongated testis.
Results and Dicsussion
The clinical presentation of complete epididymotesticular non-union can vary widely. In Case 1, the initial suspicion of a hydrocoele led to further investigations, revealing a cryptorchid left testis with an epididymotesticular non-union. In Case 2, the patient presented with cryptorchidism, and laparoscopic exploration revealed the dissociation of the vas deferens from the testis. Case 3 involved a patient with an atrophic left testis, initially presumed to be hypotrophic due to cryptorchidism but later confirmed as an epididymotesticular non-union.
These cases emphasize the importance of a comprehensive evaluation in patients with suspected TEFA. A thorough clinical examination, including scrotal ultrasound and, if necessary, laparoscopic exploration, for accurate diagnosis and treatment planning. Scrotal ultrasound is a valuable tool in diagnosing TEFA. It allows for the visualization of testicular position, size, and associated abnormalities. Laparoscopic exploration, as seen in Case 2, is essential for cases where the diagnosis is uncertain or when surgical intervention is planned. It provides direct visualization of the testis and its anatomical relationships, aiding in the decision-making process regarding orchidopexy or orchidectomy The surgical management of complete epididymotesticular non-union requires an individualized approach based on the specific case presentation. The choice between orchidopexy and orchidectomy depends on factors such as testicular viability and mobility.
The surgical management of complete epididymo-testicular non-union requires an individualized approach based on the specific case presentation. The choice between orchidopexy and orchidectomy depends on factors such as testicular viability and mobility.
These 3 cases emphasize that when encountering nonpalpable testis cases where the vas deferens and epididymis extend to the scrotum, the possibility of an intra-abdominal testis due to a non-union phenomenon should be taken into consideration. In such situations, it is necessary to conduct an extended surgical exploration to thoroughly investigate the condition instead of relying solely on ultrasound imaging [1,4- 6]. The anatomopathological findings in all three cases confirmed the presence of epididymo-testicular nonunion and excluded malignancy. Further studies and long-term follow-up are necessary to evaluate the longtestis term effects of surgical interventions and their impact on testicular function and fertility potential in patients with complete epididymo-testicular non-union.
Conclusion
Complete epididymo-testicular non-union can manifest in diverse ways, necessitating comprehensive evaluations comprising clinical examination, scrotal ultrasound, and laparoscopic exploration when needed. This case-report emphasizes the need for individualized surgical management, considering testicular viability and mobility. Long-term follow-up will be essential to assess the effects of surgical interventions on testicular function and fertility potential in these patients.
References
- Karaman A, Karaman I, Yılmaz E, et al. Complete urogenital nonunion. J Pediatr Surg. 2011; 46(12):e17-e18.
[Crossref] [Google Scholar] [PubMed]
- Qin KR, Morley C, Nataraja RM, et al. The spectrum of testicular-epididymal fusion anomalies in children with cryptorchidism: Personal experience, systematic review and meta-analysis. J Pediatr Urol. 2020; 16(2):124-129.
[Crossref] [Google Scholar] [PubMed]
- Joseph A, Yao H, Hinton BT. Development and morphogenesis of the Wolffian/epididymal duct, more twists and turns. Dev Biol. 2009; 325(1):6-14.
[Crossref] [Google Scholar] [PubMed]
- Foley PT, Sparnon AL, Lipsett J. Urogenital nonunion--the case for laparoscopy for the impalpable testis. Pediatr Surg Int. 2005; 21(8):655-656.
[Crossref] [Google Scholar] [PubMed]
- Wiese CB, Deal KK, Ireland SJ, et al. Migration pathways of sacral neural crest during development of lower urogenital tract innervation. Dev Biol. 2017; 429(1):356-369.
[Crossref] [Google Scholar] [PubMed]
- Ergashev K, Chung JM, Lee SD. Concealed index for concealed penis in prepubertal children. Investig Clin Urol. 2021; 62(2):217-213.
[Crossref] [Google Scholar] [PubMed]
Author Info
Stijn van Sas*Received: 11-Oct-2023, Manuscript No. PUCR-23- 116313; , Pre QC No. PUCR-23- 116313; Editor assigned: 16-Oct-2023, Pre QC No. PUCR-23- 116313; Reviewed: 30-Oct-2023, QC No. PUCR-23- 116313; Revised: 06-Nov-2023, Manuscript No. PUCR-23- 116313; Published: 13-Nov-2023, DOI: 10.14534/j-pucr.20222675608
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.