Case Report - (2021) Volume 8, Issue 3
An extremely rare case of diphallia with high anorectal malformation with perineal lipoma
Jiledar Rawat, Sudhir Singh*, Nitin Pant and Survesh Kumar GuptaAbstract
Diphallia is a very rare congenital anomalies occurs 1: 5-6 Million live birth. Associated anomalies like imperforate anus, vertebral deformities, double bladder, exstrophy of the cloacae, and duplication of the recto sigmoid may occurs in association with this. Amongst all anorectal malformations is a common congenital anomaly that can occur in association with diphallia. Here we are presenting a neonate with double functional penis, partial scrotal dysraphism, high anorectal malformations, presence of spina bifida occulta and a perineal lipoma successfully managed by us at our center
Keywords
Diphallia, anorectal malformations, neonate
Introduction
Diphallia is a very rare congenital anomalies occurs 1: 5-6 Million live birth in the United States [1]. In India the exact incidence is not known. The first case was reported in 1609 by Wecker, in Bologna, Italy [2]. Since then upto 110 cases have been reported in the literature. This condition has existed in humans since ancient times. Based on the presence of one or two corpora cavernosa in each phallus, diphallia is respectively defined as bifid phallus and true diphallia. Here we are reporting a case of true diphallia with high anorectal malformations, perineal lipoma and spina bifida occulta. In this case successful staged reconstruction was done.
Case History
A neonate presented to us on day two of life with complaints of not passing stool, abdominal distention, had two penises and passing urine from both. The baby delivered from 30 years old prime mother with no antenatal complains, with no history of consanguinity of the parents, antenatal checkup and ultrasound was normal. On examination of baby mild hypothermia, tachycardia and dehydration was present. Abdomen was distended and soft, on perineal examination anal opening was absent, no perineal meconium stain or fistula found. A small 2.5 × 2.5 cm perineal lipoma was found. Though the scrotum was single with well-developed rouge and two testes palpable in it however there were two median raphes (Fig 1). There was no urinary dribbling. There were two well form penis present side by side and on passing the feeding tube both penises had patent urethra with urine coming out from it. On examination of spine though externally looking normal but on palpation lower lumber spinous process not palpable, suggested features of spina bifida occulta. The movement in bilateral lower limb was normal and there were no limb deformity was present. The baby was stabilized with intravenous fluid, warmer care, oxygen started by hood and broad spectrum antibiotic started. The baby evaluated with cross table prone lateral X-ray pelvis, suggested high anorectal malformation, ultrasonography of spine suggested two hemi cords separated by a fibrous septum and reside in two separate dural tubes and ultrasonography of urinary system suggested normal upper tract and bladder. Baby was managed with high sigmoid colostomy under general anesthesia. Intraoperatively no other anomalies of hindgut found. Postoperative recovery was uneventful. Distal colostogram suggest no urinary fistula and micturating cystourethrogram suggest single bladder with duplication of urethra below bladder neck, both urethras looking good caliber (Fig 2).
At age of six months baby was readmitted for further reconstruction. Pre-anesthetics blood investigations were found with in normal range. Karyotyping study showed 46XY. Ultrasonography of upper urinary system and echocardiography were found normal. Under general anesthesia excision of left less developed penis, closer of left urethral stump closer to its origin from right urethra, excision of perineal lipoma and posterior sagittal anorectoplasty along with scrotal reconstruction was done. Postoperatively baby done well. Sigmoid colostomy closer done after two months. Now baby is doing well 10 months in follow up with continent for urine and feces.
Results and Discussion
In diphallia the two external genitalia may vary in size and shape, either lying beside each other in a sagittal plane or one above the other, no two cases have been identical. According to Schneider classification, double penis is classified into three groups: glans diphallia, bifid diphallia and complete diphallia (double penis) [1- 3]. According to Vilanora and Raventos, a fourth group called pseudodiphallia is added in which small accessory penile-like tissue is found [4]. The current widely accepted classification, introduced by Aleem, classifies double penis into two groups: true diphallia and bifid phallus [5]. True diphallia is caused by cleavage of pubic tubercle; bifid phallus is caused by separation of pubic tubercle. Each of these two groups is further subdivided into partial or complete. True diphallia is where each phallus has two corpora cavernosa and a single corpus spongiosum containing a urethra. In bifid phallus, each phallus has only one corpus cavernosum and one corpus spongiosum containing a urethra. Diphallia occurs in the fetus in fourth week of gestation by various possible embryological causes suggested are incompletely fused bilateral anlagen or a form of atavism, due to inhibited growth of the dorsal inferior wall of the urogenital sinus underlay accessory urethral development [6-8]. Another theory suggest that abnormal Mullerian duct termination was responsible for urethral duplication [9]. Theory suggested by Hollowell et. al. diphallia results from the failure of fusion of mesodermal bands [10]. Another theory attributed it to an ischemic process in embryogenesis [11]. In Troyer theory, diphallia is due to mal development of the distal portion of the urethra is because of the uncoordinated growth of the urogenital sinus and the urethral plate [12]. Other systemic anomalies occurs in association with diphallia is due to a defect in connecting the genital tubercle. Urine may pass by one or both penises, as in our case coming from both penises and baby was continent. Scrotum may be normal or bifid. In our case bladder and rectum are single, the duplication of urethra occurred just below the bladder neck as seen in contrast study (Fig 2). Complete diphallus is best treated by excision of the less well developed penile structure and its urethra. In this case we found a complete duplication of the penis with two corporal bodies in each shaft and normally located meatuses. They voided clear forcible urine simultaneously. We manage the case in stage wise procedure. Initial procedure was done only diverting sigmoid colostomy to cover come the surgical emergency of intestinal obstruction. We did posterior sagittal anorectoplasty and excision of left penis and perineal lipoma with reconstruction of scrotum in second stage of procedure. Amputation of accessory penis along with urethral end- to-side anastomosis in anterior urethra can be an option as done by some, we only remove the accessory penis with closer of urethral stump close to its bifurcation from main right urethra as in Fig 2, we can see that the course of right urethra is straight, left urethra is looking as originate as a branching from right main urethra below bladder neck [13,14]. On review of the literature, we did not come across any other case of this variety of the penile duplication with anorectal malformations.
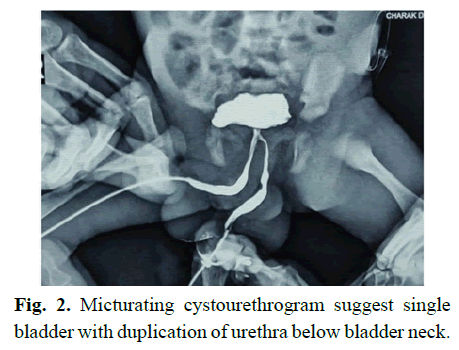
Fig. 1. Absence of anal opening with perineal lipoma, two median raphes on scrotum. Two well form penis side by side.
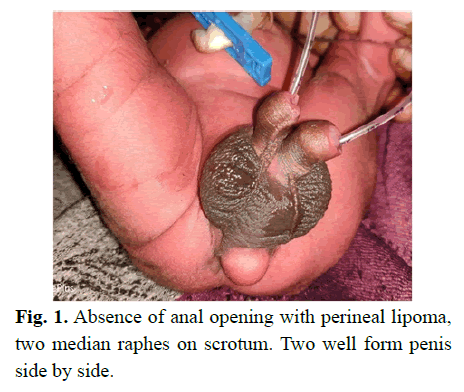
Fig. 2. Micturating cystourethrogram suggest single bladder with duplication of urethra below bladder neck.
Conclusion
Diphallia is a very rare congenital anomaly can occurs in association with anorectal malformations. Managements of such cases should be individualized on the basis of the severity and spectrum of anomalies.
Compliance with ethical statements
Conflicts of Interest: None.
Financial disclosure: None.
Consent: Patient confidentiality has been maintained and written consent has been obtained from the patient’s parents for the publication of patient information and clinical pictures and can be provided as required.
References
- Tirtayasa PMW, Prasetyo RB, Rodjani A. Diphallia with associated anomalies: A case report and literature review. Case Rep Urol. 2013; 2013: 192960
- Wecker S. Pene gemino visus quidam. Obs Med. Admirab Lib. De partibusgenitalibus, Francoforti 1609.
- Schneider P, Lattimer JK, Uson AC. The male genital tract. In: Mustard WT, Ravitch MM, Synder WH, Welch K, Benson CD, eds. Pediatric surgery. 2nd edn Chicago: Year Book Medical Publishers, 1969:1163
- Vilanova X, Raventos A. Pseudodiphallia, a rare anomaly. Urology. 1954; 71: 338–46.
- Aleem AA. Diphallia: report of a case. J Urol 1972; 108: 357–8.
- Kundal VK, Gajdhar M, Shukla AK, Kundal R. A rare case of isolated complete diphallia and review of the literature. BMJ Case Rep. 2013; bcr2012008117
- Cecil AB. Anatomy, anomalies and injuries of the penis. In: Cabot H, ed. Modern urology. Philadelphia, PA: Lea and Febiger, 1936:162.
- De vries PA, Friedland GW. Congenital ‘H-type’ anourethral fistula. Radiology1974; 113:397.
- Das S, Brosman SA. Duplication of the male urethra. J Urol 1977; 117:452.
- Hollowell JG, Witherington R, Ballayas AJ. Embryologic considerations of diphallusand associated anomalies. J Urol 1977; 117:728–32.
- Woodhouse CRJ, Williams DI. Duplications of the lower urinary tract in children. Br J Urol 1979; 51:481.
- Troyer JR. Urethral duplications. Dial Pediatr Urol 1987; 10:2.
- Karagözlü Akgül A, Uçar M, Çelik F, Kırıştıoğlu I, Kılıç N. Complete penile duplication with structurally normal penises: A case report. Balkan Med J. 2018; 35:340-43.
- Deshpande V. Complete diphallia – Our technique to avoid complications. J Indian Assoc Pediatr Surg 2020; 25:182-3.
Author Info
Jiledar Rawat, Sudhir Singh*, Nitin Pant and Survesh Kumar GuptaReceived: 12-Apr-2021 Accepted: 26-Apr-2021 Published: 03-May-2021, DOI: 10.14534/j-pucr.2021267549
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
