Case Report - (2023) Volume 10, Issue 1
Congenital Pseudo Diphallia-A rare case presentation
Amit Kumar Mishra*Abstract
References
Best Betting Sites in Turkey Blog | Mexican Food Recipes Casino Sites in Argentina Best Betting Sites in Canada Blog | Turkish Food Recipes Fan Tokens Info Blog | Vietnamese Food Recipes Engine Technologies Articles Blog | Yacht Charter in UAE All About Digital Coins Blog | Yacht Charter in Balkans Casino Sites in Bangladesh Blog | Yacht Charter in Australia Mortgage info in New York Blog | Yacht Charter in China Best Betting Sites in Nigeria Blog | Yacht Charter in Spain Best Betting Sites in United Arab Emirates Blog | Yacht Charter in France Places to Visit in ChinaIntroduction
Diphallia or penile duplication is an extremely uncommon congenital anomaly, incidence being 1/ five to six million new births [1,2]. Despite being a rarity the severity of confirmed cases have myriad presentation ranging from just a small accessory penis like appendage on one end of spectrum to complete true penile duplication on other extreme end which may or may not be associated with concommittant anomalies of urogenital, musculoskeletal and gastrointestinal systems [3]. In contrast to True Diphallia, Pseudodiphallia is further more rarity than former itself, usually presenting as a small accessory penile like structure without a normal complete internal penile anatomy. Pseudodiphallia patients usually do not have associated ureteral, renal or any other congenital malformations [4, 5]. We present such a case encountered by us of Pseudodiphallia. Despite being known since 17th century {Wecker in 1609} there has been slightly more than 100 cases reported so far. There is paucity of published work on the current topic, but we reviewed the literature to have a depth of embryology, etiology, classification and surgical techniques for penile duplication.
Case Presentation
A 5.5 year old male child was brought to the paediatric surgery OPD by the parents with complaint of difficulty in retracting the pre pucial fore skin and presence of some growth near the glans. There was no other complaints in specific.
Child was youngest of the two siblings of their parents, elder one being a girl child 3 years older, in perfect state of health and wellbeing. He is a product of nonconsanguineous marriage. He was a full term lower segment caesarean section executed successfully at local hospital, with birth weight of 3 Kilogram. Postnatal both immediate and later was unremarkable.
Child has normal developmental milestones, comparable with healthy peers. There has had been no history of any prolonged illnesses or frequent hospitalisations or recurrent clinic visits. Child has had up to date vaccinations as per norms.
Clinical examination revealed fore skin retractable with difficulty and small conical lump smaller than original glans approximately size ~1cm diameter at base attached horizontally at left side of the original glans at the coronal sulcus and visible incomplete clefting in between the 2 glans visible from the aerial view. The additional lump was visible only on full retraction of the prepucial skin. The lateral lump has had no opening or dimple or fossa at its apex. Child used to pass urine from the urethral meatus situated at navicular fossa of the central large glans. On rolling back the prepucial, the covered phallus was externally almost normal and unremarkable in size and appearance. There were no complaints of any deviation of penis or any pain or discharge. Bilateral testes were normally palpable in the scrotum, and there was no inguino scrotal swelling or lump present.
Patient was admitted, investigated, treated symptomatically.
Results
Haemoglobin 11.3gm%, Total count 13,270/cmm, differential count, platelet count 3,82,000/cmm, blood sugar 80 mg%, SGOT SGPT 38U/Serum creatinine 0.3mg%, normal serum electrolytes and bilirubin, non-reactive viral markers.
Pre-operative status
After approval from anesthetist the patient was operated under general anesthesia by excision of pseudodiphallia (Figure 1). Urethral catheterization and circumcision of penis after taking informed parental consent. Excised lump was sent for histopathological examination. Small aseptic dressing with infant feeding tube of small size as an indwelling urinary catheter was continued (Figure 2).
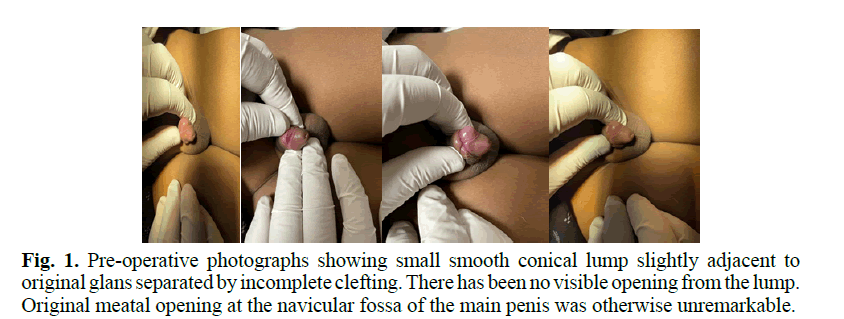
Fig. 1. Pre-operative photographs showing small smooth conical lump slightly adjacent to original glans separated by incomplete clefting. There has been no visible opening from the lump. Original meatal opening at the navicular fossa of the main penis was otherwise unremarkable.
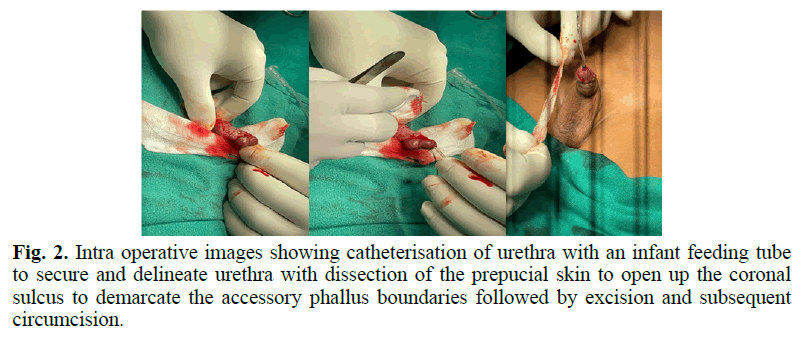
Fig. 2. Intra operative images showing catheterisation of urethra with an infant feeding tube to secure and delineate urethra with dissection of the prepucial skin to open up the coronal sulcus to demarcate the accessory phallus boundaries followed by excision and subsequent circumcision.
Post-operative status
Post operatively period was uneventful. Patient responded well to the symptomatic treatment and was orally allowed on the same day evening. Urinary catheter was removed on 5th post-operative day. The patient was discharged on oral symptomatic medication and was adviced for follow up (Figures 3 and 4).

Fig. 3. immediate post-operative period.
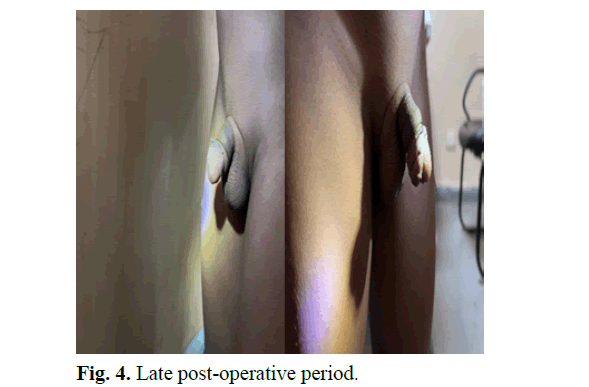
Fig. 4. Late post-operative period.
Histopathology report
Excised tissue sent for histopathological examination revealed pictures tissue partly lined by keratinised stratified squamous epithelium. Sub epithelium shows fibro connective tissue with focal areas of inflammatory infiltrate comprising of lymphocytes, plasma cells, neutrophils (Figure 5).
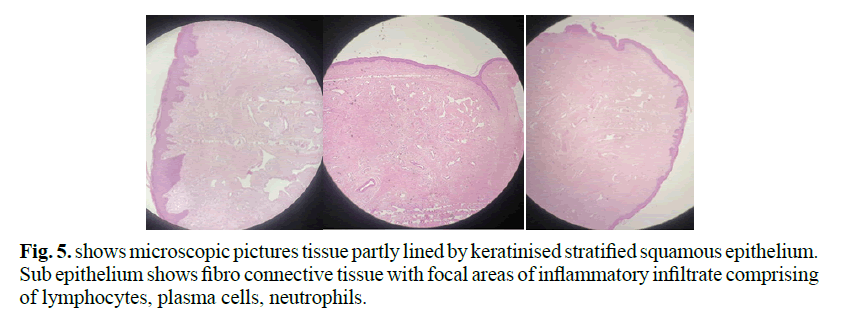
Fig. 5. shows microscopic pictures tissue partly lined by keratinised stratified squamous epithelium. Sub epithelium shows fibro connective tissue with focal areas of inflammatory infiltrate comprising of lymphocytes, plasma cells, neutrophils.
Follow up
Patient remained complaint free at home and was able to attend the nature’s call on its own unaided. In the follow up, the surgical wound has healed fully and the patient was having almost a normal looking penis with normal functioning as in ab-intio pre-operative level.
Discussion
Penile duplication, also known as diphallia, is a very rare congenital anomaly with an incidence of 1 in 5 to 1 in 6 million live births. Congenital malformations that do not clearly fit into recognised congenital anomaly syndromes can occur as sporadic or isolated cases, as part of a constellation of multiple systems, or in combination with other conditions. Although uncommon, the severity of confirmed cases can present in a variety of ways, from a small accessory penis-like appendage on one extreme to a complete true penile duplication on the other. Concomitant urogenital anomalies like renal anomalies may or may not be present, ectopic kidney, horse shoe kidney, bladder exstrophy or bladder duplication hypospadias, musculoskeletal like pubic diastasis, lumbosacral anomalies and gastrointestinal systems like imperforate anus. Pseudophallia, in contrast to True Diphallia, is even more uncommon than the former; it typically manifests as a small accessory penile-like structure without a typical complete internal penile anatomy. Patients with pseudodiphallia typically do not have any associated renal, ureteral, or other congenital malformations.
Cases associated with complete duplication with or without associated other systems anomalies present as a surgical challenge, mandating multiple surgeries or staged procedures. The normal development of penis begins when the bilateral cloacal tubercles start coalescing at the anterior end of the pars phallica of the urogenital sinus. Columns of mesoderm growing rapidly around the lateral margins of the cloacal plate form the genital tubercle. These mesodermal bands arise from more than one area and failure of these bands to fuse is expected to result in bladder exstrophy and split penis, but not true diphallia, thereby giving rise to assumptions that additional steps are needed for complete penile duplication. Probably a longitudinal duplication of cloacal membrane would permit 3 or 4 columns of primitive streak mesoderm to migrate ventrally around the two cloacal membranes to eventually form two genital tubercles culminating in collateral urethral duplication. Such Duplication of cloacal membrane could also explain the frequent concomitant bladder, colon, anal, and spinal anomalies [2-5]. One school of thought presumes 3-5 weeks of gestation as optimal time for diphallia to set in during embryogenesis. The other thinkers presume that anomalies take place in the process of migration ventrally and fusion of the paired mesodermal anlage by the 15th week of gestation [4]. The exact mechanism during embryogenesis leading to penile duplication is not certain, as genital tubercle is believed to arise as a single structure, however but can be understood by defined time frame alterations leading to this viz. (i) pubic tubercle separation during embryogenesis resulting in gain of one corpora and one urethra by each phallus, or (ii) cleavage of pubic tubercle leading to each phallus gaining 2 corporal bodies and urethra. Almost all authors agree that the anomaly is due to a defective fusion of the genital tubercle [2, 3]. Current common consensus is that the penile duplication is a result of lack of fusion of the paired mesodermal anlagen of the genital tubercle by the 15th week of gestation [6, 7].
Diphallia being a rare occurrence, no two different cases are presumed to be identical as they are mostly sporadic, since the familial dominant variety is a rarest one.
Diphallia varies from small accessory penis or glans duplication on one end to complete penile duplication on other. Penile duplication may be orthotropic or ectopic. Penile division may be sagittal or frontal and symmetric or asymmetric, in shape and size [1, 3]. Schneider had divided diphallia into 3 groups’ isolated diphallia of the glans alone, bifid diphallia, and complete diphallia. Villanova and Raventos added a fourth category, pseudodiphallia. The urethra shows a range of variations, from functioning double urethras to complete absence of the urethra in each penis [2]. The majority have a single corpus cavernosum in each organ. The meatus may be normal, hypospadias, or epispadia, and the scrotum may be normal or bifid. The testes are normal, athropic, or undescended [2, 4]. The most commonly accepted classification for urethral duplication anomalies is described by Effmann et al. Almost all karyotype analyses of patients diagnosed with diphallia are found to be normal.
Gyftopoulos et al. has proposed a classification dividing cases into 2 broad categories: True diphallia and Bifid phallus. Both groups can be further sub classified into partial or complete duplication. True complete diphallia will have 2 well-developed penises (with 2 corpora cavernosa and 1 corpora spongiosum). True partial diphallia will have a smaller or rudimentary duplicate penis (with complete structures that is 2 corpora cavernosa and 1 corpora spongiosum). If the duplicate penis does not have all the structures, for example one corpora cavernosum they are classified as bifid phallus. Depending on the degree of separation, bifid phallus is further sub classified into complete and partial. Complete bifid phallus has separation at the base whereas; partial bifid phallus has separation at the glans. When the degree of separation is complete to the base of the shaft or to just the glans, the anomaly is considered complete or partial bifid phallus, respectively. The term “pseudodiphallia,” as originally described by Villanova and Raventos, corresponds to true, partial diphallia [3, 5].
Treatment requires correct diagnosis by imaging techniques starting from ultrasound of abdomen and genitalia, with adjuncts from other modalities like contrast Computerised Tomographic Scan (CECT), Magnetic Resonance Imaging (MRI), Micturating Cystourethrogram (MCU), and Retrograde Uretherogram (RGU) in difficult cases. Treatment planning needs to address ethical medical and cosmetic/ aesthetic issues. Once the corporal development and urethral anatomy is delineated by history, clinical and radiological assessment, classifying the degree of penile duplication to decide the treatment of excision or reconstruction of duplicated penis.
Conclusion
Since the presentation is extremely rare, hence one needs to have a high index of suspicion to have had early diagnosis in ambiguous cases. Patients have had different presentations and therefore each patient requires a separate individualised tailor made approach taking into account both the penile as well as associated anomalies to get a satisfactory outcome. In pseudodiphallia the rudimentary phallus is rarely functional, making excision decision easy.
Early treatment is advised with the aim of obtaining a cosmetically acceptable/ appeasing and optimally functioning (both erectile and voiding functions) penis. Treatment usually involves removal of less or non-functioning, non-communicating or accessory phallus. Since no two cases are identical hence individualised treatment is required considering the type of diphallia and accompanying abnormality to finalise a surgical remedy which aims at preserving urinary continence, erectile function, optimum urinary stream and perfect cosmesis.
References
- Karagozlü AA, Uçar M, Çelik F, et al. Complete penile duplication with structurally normal penises: a case report. Balkan Med J. 2018;35(4):340-343.
[Crossref] [Google Scholar] [PubMed]
- Bhat HS, Sukumar S, Nair TB. Successful surgical correction of true diphallia, scrotal duplication, and associated hypospadias. J Pediatr Surg. 2006;41:13-14.
[Crossref] [Google Scholar] [PubMed]
- Gyftopoulos K, Wolffenbuttel KP, Nıjman RJ. Clinical and embryologic aspects of penile duplication and associated anomalies. Urology. 2002;60:675-679.
[Crossref] [Google Scholar] [PubMed]
- Gupta M, Virdi VJS. Rare case of isolated true complete diphallus – case report and review of literature. SAS J. Surg. 2016:23-25.
- M. E. Torres, P. J. C. Sanchez, T. A. Aragon, et al. Diphalia Revista Mexicana de Urolog´ıa. 2009;32-35.
- Stephans FD, Smith ED, Hutson JM. Congenital Anomalies of the Urinary and Genital Tracts. Oxford: Isis Medical Media. 1996:83-84.
- Hollowell JG, Witherington R, Ballayas AJ. Embryologic considerations of diphallus and associated anomalies. J Urol. 1977; 117:728-732.
[Crossref] [Google Scholar] [PubMed]
Author Info
Amit Kumar Mishra*Received: 27-Jan-2023, Manuscript No. PUCR-23-88075; , Pre QC No. PUCR-23-88075 (PQ); Editor assigned: 30-Jan-2023, Pre QC No. PUCR-23-88075 (PQ); Reviewed: 10-Feb-2023, QC No. PUCR-23-88075; Revised: 17-Feb-2023, Manuscript No. PUCR-23-88075 (R); Published: 27-Feb-2023, DOI: 10.14534/j-pucr.20222675598
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
