Case Report - (2024) Volume 11, Issue 5
Exit strategy in extensive urological involvement by epidermolysis bullosa: A case report
Ganesh Vythilingam1,3, Eleni Papageorgiou2, Usman Ali3 and Abraham Cherian3*Abstract
Epidermolysis Bullosa (EB) is a rare, inherited skin disorder, characterized by marked mechanical fragility of epithelial tissues and continuous development of non-inflammatory blisters. We present the management of a child with extensive EB of the genitourinary system and a brief review of our experience with the management of urological complications in EB patients. An 11-year-old Ex Prem 29/40, EB-Junctional type with multiple co-morbidities and bilateral end ureterostomies had persistent bilateral hydroureteronephrosis, recurrent UTI, and worsening CKD. The disease extensively involved the urethra, bladder and ureter. The entire ureter on the right, and two thirds of the ureter on the left were substituted using an integrated ileal conduit with augmentation cystoplasty using the “FEZ” technique. A posterior appendix mitrofanoff was also fashioned in the midline. The patient is well 2-years post-surgery. Twenty patients with EB were identified to have urological involvement in our institution between 1986-2022. The severity of the urological involvement in patients with EB was significantly associated with the EB-type (Fisher-test: p=0.035). Interventions and intubations of the urinary tract must be very carefully considered in genitourinary EB. At times a major reconstruction will be required and provides a much better pragmatic solution as seen in our patient.
Keywords
Epidermolysis bullosa, pediatric urology, reconstructive urology, ureteric substitution, cystoplasty
Introduction
Epidermolysis Bullosa (EB) is a rare, inherited skin disorder, characterized by marked mechanical fragility of epithelial tissues and continuous development of non-inflammatory blisters. It encompasses 4 major groups of diseases, EB Simplex (EBS), Junctional EB (JEB), Dystrophic EB (DEB), and kindler syndrome. Each of the subtypes is defined by its mode of transmission and a combination of phenotypic, ultrastructural, immunohistochemical and molecular findings. EB may manifest systemically and can involve the epithelial lining of the respiratory, gastrointestinal, and genitourinary systems, associated with complications. Some forms of Epidermolysis Bullosa (EB) are particularly susceptible to stenosis or obstruction of the genitourinary tract [1]. We present the management of a child with extensive EB of the genitourinary system and a brief review of our experience with the management of these patients with urinary tract involvement.
Case Presentation
A male, 2-year-old (2013), ex-premature with the diagnosis of junctional EB presented to our institution with bilateral hydroureteronephrosis and a left end ureterostomy. At our centre the ureterostomy was revised, and a right loop ureterostomy fashioned. Both ureters were noted intraoperatively to be of lead pipe consistency. Five years later due to ongoing stomal stenosis, the right loop ureterostomy was refashioned as an end ureterostomy. Evaluation at that time showed that the disease involved both his bladder and urethra. Recurrent Urinary Tract Infections (UTI) continued to be an issue due to poor drainage form the right side which improved with intermittent catheterisation through the ureterostomy. At the age of 11-years he and his family expressed the desire for a definitive procedure to make him dry and prevent infections. A repeat ultrasound showed persistent bilateral hydroureteronephrosis and DMSA showed new scarring. He had several co-morbidities weighing only 19.3 kg with poor dentition, anaemia with dystrophic nails and skin lesions with right eye ptosis. He had also developed other issues, some related to EB such as laryngeal stenosis and others such as diaphragmatic hernia, gastro-oesophageal reflux disease that required a fundoplication and a gastrostomy, pan colitis and finally G6PD deficiency. His clinical condition, nutritional status, co-morbidities for anaesthesia along with the extent of his genitourinary involvement led to extensive discussions in the multidisciplinary team meeting preparing for reconstructive surgery. The gastroenterology team confirmed normal small bowel, important for its utilization in the planned urinary tract reconstruction. Airway assessment was done along with laryngeal dilatation by ENT and anaesthetic team prior to elective surgery. Patient was optimized nutritionally and reviewed by dermatology and dentistry. All precautions as per our established guidelines for the care of patients with EB was utilized by the theatre team with regards to pressure points and drapes. Anaesthesia during surgery was undertaken utilizing a ‘no touch’ principle avoiding the use of any adhesive dressing. Induction using inhalational anaesthesia and an uncuffed 4.5 Fr endotracheal tube utilized as planned. A midline laparotomy revealed extensive adhesions with a small fibrotic bladder. Both ureterostomies were taken down and diseased ureter on the right was up to the Pelvic Ureteric Junction (PUJ) (Fig 1) and on the left, the upper third of the ureter was spared (Fig 2). A schematic representation of the extensive ureteric involvement is depicted in Fig 3.
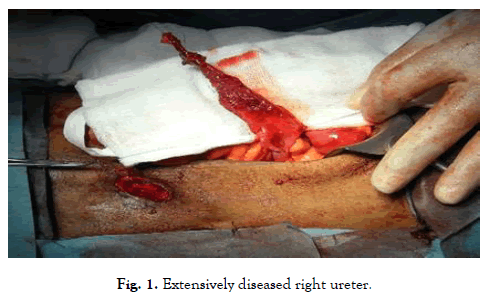
Figure 1: Extensively diseased right ureter.
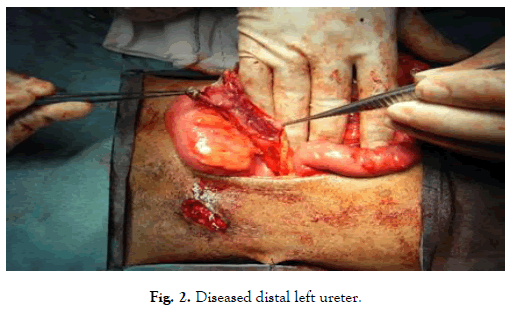
Figure 2: Diseased distal left ureter.
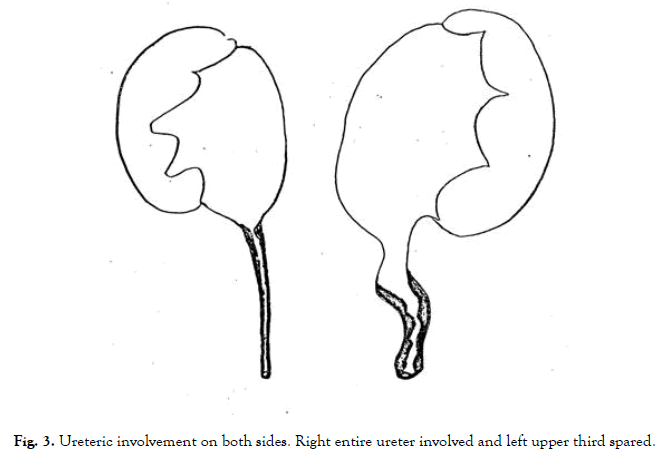
Figure 3: Ureteric involvement on both sides. Right entire ureter involved and left upper third spared.
Diseased segments of the ureter were then excised leaving the right renal pelvis and PUJ intact along with a short upper ureter on the left. The bladder was opened in the sagittal plane to create a clam configuration allowing a larger posterior wall for reimplantation of the appendix as a mitrofanoff channel. A distal ileal loop was harvested (45 cm) sparing 20 cm of terminal ileum. The isolated segment was partly (distal 30 cm) detubularised to fashion a cup patch for augmenting the bladder and the proximal 15 cm of the same segment (isoperistaltic) was not detubularised and used as an interposition conduit to connect both the renal units. An end-to-end anastomosis was done between the right pelvis to the conduit (chimney) with an to end to side anastomosis for the left upper ureter. A Shanfield type anastomosis of the appendix mitrofanoff and skin stoma, formed in the midline with 12 Fr Jacques catheter in-situ as both iliac fossae had previous ureterostomy sites. An additional 12 Fr Foley catheter suprapubic was left in place. The final configuration of the reconstruction is depicted in Fig 4.
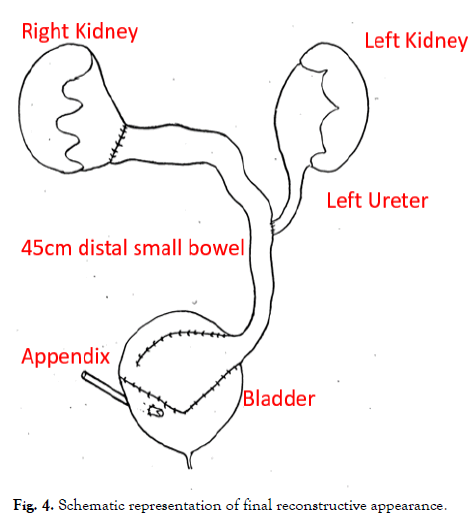
Figure 4: Schematic representation of final reconstructive appearance.
Patient made an uneventful post-operative recovery and CIC was established by a month’s time. Histology of the excised specimens was consistent with extensive fibrosis. Two-year post-surgery patient is well and independently undertaking self-catheterization with no complications.
Discussion
Genitourinary involvement of EB is rare but can be quite challenging to deal with, as patients seem to be predisposed to stenosis or obstruction of the urinary tract. They typically present with dysuria, recurrent urinary tract infections or poor urinary flow. The first report of genitourinary involvement in an EB patient was by Kretkowsk in 1973 [2]. With institutional approval, we retrospectively reviewed all EB patients in our institution with urological problems between 1986-2022. We classified the patients into two subgroups. Group A included those with specialist urinary tract diagnoses and Group B those presenting with general urological diagnoses of childhood. Statistical analysis using Fisher-test was used. Twenty patients with EB were identified to have urological involvement (Tab. 1).
| Group A: Specialist urinary tract diagnosis | Group B: General urology of childhood | ||
|---|---|---|---|
| Hypospadias | 2 | Hydrocele /Undescended testis/Testicular torsion | 3 |
| Hydroureteronephrosis (HUN) | 2 | ||
| HUN + Bladder Outlet Obstruction (BOO) | 2 | Enuresis/Bladder dysfunction-constipation | 2 |
| HUN + BOO + Renal impairment | 1 | ||
| PUV | 1 | Circumcision | 7 |
| Total | 8 | Total | 12 |
Tab. 1. Urological Involvement of EB patients divided into specialist urinary tract diagnoses and general urological diagnoses of childhood.
The severity of the urological involvement was significantly associated with the EB-type (Fisher-test: p=0.035), with six (75%) patients in Group A having JEB and two (25%) having DEB. On the contrary all three patients with EBS presented with non-specific urological symptoms of the childhood. A detailed review of genitourinary complications from the American National EB Registry had similar conclusions that urological problems are often seen in patients with more severe subtypes; JEB and DEB-variant [3-4]. In our centre’s prior publication, we had concluded that unnecessary operations be avoided, however for patients that do require intervention, it is important to recognize that anaesthesia can be potentially risky [5]. Airway management can be challenging due to the fragility of the mucosa. Patients with EB require maximal skin and mucous membrane protection. The temperature of the room, the kind of thermometers and dressings used, the blood pressure monitoring, as well as the skin swabs should all be regulated with the aim to maintain the skin integrity and avoid blistering [6]. Intraoperatively we found extensive disease involvement of his urethra, bladder, and both ureters. Mucosal surfaces in the urethra or the interface at the vesico-ureteric junctions are particularly prone to stenosis [7]. In our patient, we believe the subepithelial separation of the urothelium exposing the detrusor muscle to urine, also resulted in chronic inflammation and fibrosis of the bladder wall [8]. Based on the intraoperative findings we opted for the integrated augmentation ileocystoplasty technique called the “fez procedure” [9]. This was originally described for the management of non-compliant bladders with obstructed megaureters. The technique involves the creation of an isoperistaltic bilateral ureteric substitution with an integrated augmentation cystoplasty and an appendix mitrofanoff (Fig 4). At two years follow up, catheterization poses no difficulty with upper tracts draining well and no UTI. Literature suggests any form of active surgical intervention should be avoided in EB and if instrumentation of the urogenital tract is required, the smallest calibre instruments possible should be used to avoid injury. In our patient, extensive urinary tract reconstruction was inevitable and resulted in a good clinical outcome. Though EB does manifest with gastrointestinal pathologies, small bowel is usually spared thus making it an ideal tissue for reconstructive surgery [10]. Similar results have also been described by others who have used small bowel to reconstruct the urinary system [5,11]. Published guidelines for the treatment and follow up patients with EB is lacking.
Considering the potential urological involvement and to detect complications and treat them early, we propose a baseline urinary tract assessment is essential, especially in patients with JEB and recessive DEB. Further imaging, blood pressure measurements and renal biochemistry might be necessary, according to clinical indication When required extensive urological reconstruction using small bowel is a safe option as seen in our patient if all the necessary pre, intra and post-operative care required for EB patients is undertaken.
Conclusion
Patients with EB and genitourinary involvement is a spectrum and need a multidisciplinary approach in specialized centers. Management should be tailored to the type of EB and the degree of genitourinary involvement.
Urological complications are more commonly seen in patients with JEB and DEB subtypes. As far as possible, surgery and instrumentation of the urinary tract should be avoided. However, intervention when required should be undertaken in a planned manner and can provide patients with a better quality of life.
References
- Jesus LE, Rangel M, Moura Filho et al. Urological surgery in epidermolysis bullosa: Tactical planning for surgery and anesthesia. International Braz J Urol. 2014;40:702-707.
[Crossref] [Google Scholar] [PubMed]
- Kretkowski RC. Urinary tract involvement in epidermolysis bullosa. Pediatrics. 1973;51(5):938-941.
[Crossref] [Google Scholar] [PubMed]
- Fine JD, Johnson LB, Weiner M, et al. Genitourinary complications of inherited epidermolysis bullosa: Experience of the national epidermylosis bullosa registry and review of the literature. J Urol. 2004;172(5):2040-2044.
[Crossref] [Google Scholar] [PubMed]
- Fine JD, Bruckner-Tuderman L, Eady RA, et al. Inherited epidermolysis bullosa: Updated recommendations on diagnosis and classification. J Am Acad Dermatol. 2014;70(6):1103-1126.
[Crossref] [Google Scholar] [PubMed]
- Burgu B, Duffy PG, Wilcox DT. Single-centre experience of genitourinary complications of epidermolysis bullosa. J Pediatr Urol. 2006;2(6):583-586.
[Crossref] [Google Scholar] [PubMed]
- Ames WA, Mayou BJ, Williams KN, et al. Anaesthetic management of epidermolysis bullosa. Br J Anaesth. 1999;82(5):746-751.
[Crossref] [Google Scholar] [PubMed]
- Almaani N, Mellerio JE. Genitourinary tract involvement in epidermolysis bullosa. Dermatol Clin. 2010;28(2):343-346.
[Crossref] [Google Scholar] [PubMed]
- Reitelman C, Burbige KA, Mitchell ME, et al. The urological manifestations of epidermolysis bullosa. J Urol. 1986;136(6):1320-1322.
[Crossref] [Google Scholar] [PubMed]
- Tayib AM, Abdel‐Meguid TA, Al‐Sayyad AJ, et al. Novel augmentation ileocystoplasty technique to manage non‐compliant bladders in the presence of obstructed megaureters: The “fez procedure”. Int J Urol. 2015;22(3):301-305.
[Crossref] [Google Scholar] [PubMed]
- Fine JD, Mellerio JE. Extracutaneous manifestations and complications of inherited epidermolysis bullosa: Part II. Other organs. J Am Acad Dermatol. 2009;61(3):387-402.
[Crossref] [Google Scholar] [PubMed]
- Glazier DB, Zaontz MR. Epidermolysis bullosa: A review of the associated urological complications. J Urol. 1998;159(6):2122-2125.
[Crossref] [Google Scholar] [PubMed]
Author Info
Ganesh Vythilingam1,3, Eleni Papageorgiou2, Usman Ali3 and Abraham Cherian3*2Department of Paediatric Surgery and Urology, Royal Hospital for Children and Young People, Edinburgh, UK
3Department of Pediatric Urology, Great Ormond Street Hospital for Children, London, UK
Received: 09-Aug-2024, Manuscript No. PUCR-24-147587; , Pre QC No. PUCR-24-147587 (PQ); Editor assigned: 12-Aug-2024, Pre QC No. PUCR-24-147587 (PQ); Reviewed: 26-Aug-2024, QC No. PUCR-24-147587; Revised: 23-Oct-2024, Manuscript No. PUCR-24-147587 (R); Published: 30-Oct-2024, DOI: 10.14534/j-pucr.20222675670
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
