Case Report - (2021) Volume 8, Issue 3
Hydrometrocolpos secondary to persistent urogenital sinus and transverse vaginal septum: a rare congenital anomaly
Karamvir Chandel1*, Tulika Singh1, Veenu Singla1 and Rashmi Bagga2Abstract
Hydrometrocolpos is an uncommon congenital disorder consisting of cystic dilatation of the vagina and uterus, usually caused by distal obstruction. Many congenital urogenital malformations, ranging from persistent urogenital sinus to cloacal dysgenesis, may cause hydrometrocolpos. In obstructive, uterovaginal causes such as imperforate hymen, transverse vaginal septum are common etiologies. Early diagnosis in the antenatal ultrasound (USG) followed by fetal MRI is important, as this allows for early postnatal management and minimizes various secondary obstructive complications. We discuss hydrometrocolpos’ case associated with urogenital sinus and transverse vaginal septum diagnosed on antenatal USG and MRI scan and treated postnatally
http://www.oajournal.org/
http://www.journalsres.org/
http://www.journalsres.com/
http://www.journalsoa.org/
http://www.journalsoa.com/
http://www.journalsci.org/
http://www.journalres.org/
http://www.journalres.com/
http://www.journaloa.org/
http://www.journalinsights.org/
http://www.jpeerreview.org/
http://www.imedresearch.com/
http://www.imedpubjournals.com/
http://www.imedpubjournal.org/
http://www.imedjournals.org/
http://www.peerreviewedjournal.org/
http://www.peerjournals.org/
http://www.peerjournals.com/
http://www.sciencesinsight.org/
http://www.scholarresearch.com/
http://www.scholarres.org/
http://www.nutritionres.com/
http://www.gastroinsights.org/
http://www.pathologyinsights.org/
http://www.echemistry.org/
http://www.echemcentral.com/
http://www.chemistryres.com/
http://www.biochemresearch.org/
http://www.biochemjournals.com/
http://www.ebusinessjournals.org/
http://www.businessjournals.org/
http://www.peerjournal.org/
http://www.oajournalres.com/
http://www.alliedres.org/
http://www.alliedjournals.org/
http://www.alliedjournal.org/
http://www.scientificres.org/
http://www.scientificres.com/
,
https://www.mongoliannutrition.com/
https://www.nsbmb.com/
https://www.arabspp.org/
https://www.arabianmultidisciplinary.com/
https://www.italystemcell.com/
https://www.traditional-medicine.org/
https://www.episportsmedicine.org/
https://www.worldmedicalassociation.org/
https://www.silaeitaly.com/
https://www.ceramicsmedicine.org/
https://www.isaddictionmedicine.org/
https://www.europeanbionetwork.com/
https://www.aarsecp.com/
https://www.edycseg.org/
https://www.europeanneurology.org/
https://www.clinicaldermepi.com/
https://www.cardiac-society.com/
https://www.psychologicalassociation.org/
https://www.indian-psychology.com/
https://www.mongoliancardiology.org/
https://www.pediatricssociety.com/
https://www.cocrt.org/
https://www.european-aesthetic.com/
https://www.sohnsb.org/
Keywords
Hydrometrocolpos, antenatal ultrasound, pediatric
Introduction
Hydrometrocolpos is an uncommon congenital disorder consisting of cystic dilatation of vagina and uterus, usually caused by distal obstruction. In general, the prevalence of hydrometrocolpos is estimated to be less than 1 in 30000 births [1]. The anomaly is less frequent then hydrocolpos (cystic dilatation of vagina) [2]. Many congenital urogenital malformations, ranging from persistent urogenital sinus to cloacal dysgenesis may lead to these [3]. In obstructive, uterovaginal causes such as imperforate hymen, transverse vaginal septum are common etiologies [4]. Early diagnosis in the antenatal Ultrasound (USG) is important, as this allows early postnatal treatment plan for management of hydrocolpos or hydrometrocolpos and minimize various secondary obstructive complications. We discuss a case of hydrometrocolpos associated with urogenital sinus and transverse vaginal septum diagnosed on antenatal USG and MRI scan and treated postnatally, with focus on its associations, complications and possible differentials.
Case Presentation
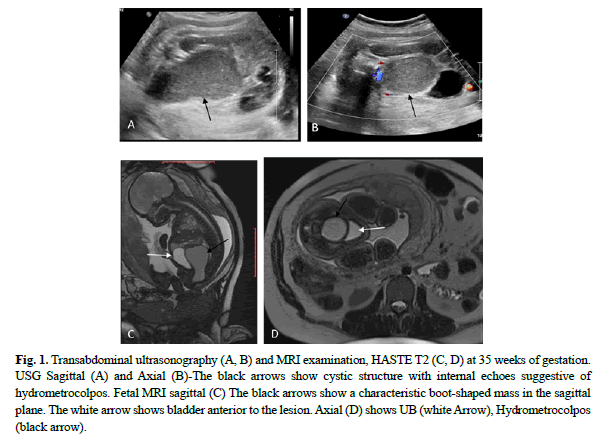
Mrs. M, 30 years old female, with h/o secondary infertility was being supervised in infertility clinic of our institute. She underwent myomectomy (15 × 15 cm, intramural, anterior wall fibroid), later conceived after intrauterine insemination. During her antenatal period, she developed Gestational Hypertension and was started on drugs. At 35 weeks of Period of Gestation (POG). On her routine Obstetric USG~4 × 3 × 5 cm hypoechoic cystic lesion was noted in fetal pelvis separate from the bladder. This was confirmed by fetal MRI and diagnosis of fetal hydrocolpos with possibility of vaginal atresia or vaginal septum was kept (Figure 1).
Fig. 1. Transabdominal ultrasonography (A, B) and MRI examination, HASTE T2 (C, D) at 35 weeks of gestation. USG Sagittal (A) and Axial (B)-The black arrows show cystic structure with internal echoes suggestive of hydrometrocolpos. Fetal MRI sagittal (C) The black arrows show a characteristic boot-shaped mass in the sagittal plane. The white arrow shows bladder anterior to the lesion. Axial (D) shows UB (white Arrow), Hydrometrocolpos (black arrow).
There was secondary compression of right ureter with right hydroureteronephrosis. Pediatric surgery consultation was taken and was planned for further evaluation and corrective procedures after birth. Patient was counseled regarding the presence of abnormal collection in the internal reproductive organs of the fetus, compressing the ureter and hydroureteronephrosis of the fetus as well as postnatal drainage or operative procedure. Patient underwent elective caesarean at 37+5 weeks POG in view of Gestational Hypertension with previous myomectomy. She delivered a baby girl, 2.3 kg with APGAR score of 8,9 at 1 and 5 min respectively. On examination of new born, per abdomen there was fullness in the lower abdomen, single opening in vestibule, normal anus, clinical impression of urogenital sinus was made. The neonate was shifted to pediatric surgery. USG abdomen and pelvis of the neonate showed, enlarged uterus and cervix, 8 × 5 × 4 cm fluid collection with hyperechoic internal echoes. No free fluid was seen in pelvis. In view of obstructive uropathy, under radiological guidance, 6F pig tail was inserted abdominally into the collection. It drained mucoid secretion around 40 ml on day 1, and 40 ml on day 2. On day 3, it drained around 15 ml of urine like secretion. Antibiotics were given. Parents were explained regarding pig tail catheter care. The neonate was discharged in stable condition and was kept under regular follow up. The drain output gradually declined to around 5-7 ml/24 hours at 6 months of age of the infant. Genitogram was done through single opening in the perineum showed opacification of linear structure which is leading into ovoid midline structure likely urethra and bladder respectively. Pigtail contrast study showed a contrast filled tubular structure in pelvis. There is presence of a transverse septum present at the distal end of the contrast filled structure. No distal passage of contrast across the septum. Definitive procedure in form of septal resection and vaginoplasty done at 6 months of age. Combined suprapubic and perineal approach used. Hydrometrocolpos identified, vagina opened and collection drained. Suprapubic incision and vagina closed in layers.
Results and Discussion
We present a case of cystic pelvis mass secondary to persistent urogenital sinus and transverse vaginal septum detected on prenatal ultrasound and MRI.
Fetal hydrometrocolpos is an uncommon disorder characterized by distension of the endometrial and vaginal cavity with fluid accumulation [3]. Increased secretions, secondary to increased stimulation of cervical and vaginal glands by maternal hormones, gradually accumulates due to distal obstruction and leads to a cystic mass in pelvis. Internal fluid debris may be noted and suggests thick mucoid secretions. Also, persistent urogenital sinus may result in fluid accumulation. This usually represents urine collection. Hence the presence of debris may also imply presence of persistent urogenital sinus [1,3]. Most of the cases of hydrometrocolpos are sporadic, but associations with other etiologies are also seen [1]. This may occur post steroid management of congenital adrenal hyperplasia [4]. It is also associated with some genetic syndromes like Bardet-Biedl, Pallister hall and McKusik-Kaufman syndromes [5]. McKusick–Kaufman syndrome is an autosomal recessive disorder with hydrometrocolpos associated with vaginal atresia, congenital heart defects, polydactyly and non-immune mediated hydrops fetalis [6].
Hydrometrocolpos usually represents a type of obstructive Mullerian anomaly. Most cases ,of hydrometrocolpos occur due to persistent urogenital sinus or cloacal malformation [4]. Persistent urogenital sinus is associated with other ano-rectal as well as urogenital malformations, such as cloacal anomaly, vaginal septum, vaginal atresia, and imperforate hymen [5]. Each of these may cause distal obstruction leading to hydrocolpos and hydrometrocolpos [3,4,7]. Urogenital sinus with transverse vaginal septum were present in our case. Vaginal septum is one of the Hydrometrocolpos usually represents a type of obstructive Mullerian anomaly. Most cases of hydrometrocolpos occur due to persistent urogenital sinus or cloacal malformation [4]. Persistent urogenital sinus is associated with other ano-rectal as well as urogenital malformations, such as cloacal anomaly, vaginal septum, vaginal atresia, and imperforate hymen [5]. Each of these may cause distal obstruction leading to hydrocolpos and hydrometrocolpos [3,4,7]. Urogenital sinus with transverse vaginal septum were present in our case. Vaginal septum is one of the common causes. It is a fibrous membrane of connective tissue with associated vascular and muscular components. It can be longitudinal, transverse or oblique. Most common in upper vagina (~46%), followed by middle vagina (~40%) and lower vagina (14%) [8].
A detailed prenatal USG, usually in third trimester is suggestive of a cystic pelvis mass. It should be evaluated further with MRI. MRI with excellent soft tissue contrast provides better additional anatomic details and the cause of distal obstruction. It also provides details of thickness of the transverse septum, length of the atresia, and the presence or absence of a cervix and vagina. [3,8].
Possible differential diagnoses of antenatal pelvic cystic mass include other presacral cystic masses like dermoid cyst, enteric cyst, ovarian cyst, sacrococcygeal teratoma, anterior sacral meningocele, cystic lymphatic malformations [1,5]. Sacrococcygeal teratoma may show internal echogenic areas suggestive of fat or debris. Dermoid cyst, a type of teratoma contains fatty or calcific components. An, anterior sacral meningocele if present is usually associated with spinal bony defects. Enteric cysts may present as unilocular or multilocular cysts, causing retro rectal space widening and may show communication with the bowel lumen. Retroperitoneal cystic lymphatic malformations are uni or multilocular cystic lesions with varying internal echogenicity [1].
Hydrometrocolpos may be associated with various complications. Bladder compression may lead to hydronephrosis, which ultimately may lead to kidney damage [2]. Others associations includes ascites [5], pyometrocolpos [6]. Timely interventions and early drainage of the cyst prevent various complications which signifies importance of early antenatal diagnosis. Definite management can be planned after proper thorough evaluation.
Conclusion
Hydrometrocolpos is a possible cause of fetal cystic pelvis mass. Transverse vaginal septum and obstructive uropathy could be associated conditions. It is important that clinicians and the radiologists should be aware of hydrometrocolpos as a cause of cystic pelvic mass and also its syndromic associations, complications and differentials for complete thorough evaluation and diagnosis. The Prenatal diagnosis lead to early detection, early management of these cases which is important to avoid secondary complications.
References
- Taori K, Krishnan V, Sharbidre KG, Andhare A, Kulkarni BR, Bopche S, et al. Prenatal sonographic diagnosis of fetal persistent urogenital sinus with congenital hydrocolpos. Ultrasound Obstet Gynecol. 2010; 36: 641-643.
- Ayaz UY, Dilli A, Api A. Ultrasonographic diagnosis of congenital hydrometrocolpos in prenatal and newborn period: A case report. Med Ultrason. 2011;13: 234-236.
- Murthy V, Costalez J, Weiner J. Two neonates with congenital hydrocolpos. Case Rep Pediatr. 2013;2013: 692504.
- Garel L, Dubois J, Grignon A. US of the pediatric female pelvis: a clinical perspective. Radiographics. 2001; 21: 1393-1407.
- Nigam A, Kumar M, Gulati S. Fetal ascites and hydrometrocolpos due to persistent urogenital sinus and cloaca: a rare congenital anomaly and review of literature. BMJ Case Rep. 2014; 2014: 22231.
- Tilahun B, Woldegebriel F, Wolde Z, Tadele H. Hydrometrocolpos presenting as a huge abdominal swelling and obstructive uropathy in a 4 day old newborn: A diagnostic challenge. Ethiop J Health Sci. 2016;26: 89-91.
- Adaletli I, Ozer H, Kurugoglu S, Emir H, Madazli R. Congenital imperforate hymen with hydrocolpos diagnosed using prenatal MRI. AJR Am J Roentgenol. 2007; 189: W23-W25.
- Abdulqader N, Alwafi B, Al-Sharief S. Case report: Transverse vaginal septum in a down’s syndrome patient. The Egyptian Journal of Hospital Medicine. 2018 1;71: 2715-7.
Author Info
Karamvir Chandel1*, Tulika Singh1, Veenu Singla1 and Rashmi Bagga22Department of Obstetrics and Gynecology, Post Graduate Institute of Medical Education and Research, Chandigarh, India
Received: 28-Apr-2021 Accepted: 12-May-2021 Published: 19-May-2021, DOI: 10.14534/j-pucr.2021267552
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.