Mini Review - (2023) Volume 10, Issue 6
Laparoscopic surgical treatment of ureterosciatic hernia after repeated recurrence despite conservative treatment: A systematic review
Takahiro Hoshino1, Takehiro Sejima1*, Hideto Iwamoto1 and Youji Fukumoto2Abstract
Ureterosciatic hernia is a rare condition in which the ureter prolapses from the foramen sciaticum. Pro- lapsed organs, other than the ureter, include the ovary, small intestine, colon, and bladder. Ureteral sciat- icum hernia is the rarest form of sciatic hernia, and causes ureteral dilation and hydronephrosis, leading to urinary tract infections and renal failure. Treatment options include surgical and conservative treat- ments with ureteral stenting; however, no consensus has been reached. Surgical treatment includes uret- eral anastomosis, uretero-bladder neoanastomosis, and mesh reinforcement of the sciatic foramen. There have been scattered reports of laparoscopic or robot-assisted repair in recent years.
In this Systematic review, we are presenting and discussing a previous case of ureterosciatic hernia treated with laparoscopic surgery after repeated recurrence despite conservative treatment, including a mini-re- view of the literature. Due to the extreme rarity of the condition, an effective and reliable long-term prognosis has not to be established yet. However, early diagnosis and appropriate target of treatment are essential for optimal recovery, especially in multiple recurred cases. During our review of the literature, to the best of our knowledge and effort, we could not find the consensus of best management of ureteros- ciatic hernia. However, surgical treatment is necessary for the case of ureterosciatic hernia that could not be cured through the conservative approach. Due to the extreme rarity of the condition, optimal surgical technique has not been established. In this mini-review, we are also presenting detailed laparoscopic sur- gical procedures to be informative for urological surgeons who will operate similar cases in the future.
Keywords
Laparoscopic surgery, Recurrence, Ureteral stent, Ureterosciatic herniaIntroduction
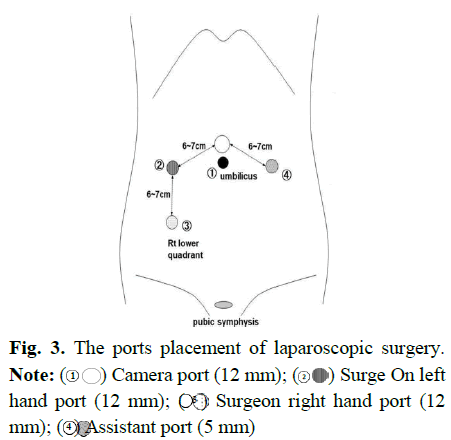
Sciatic hernia is the results as herniated contents protrude through the greater or lesser sciatic foramen. Herniated contents vary by organs, including ovary, small intestine, colon, greater omentum, or even neoplasms. Ureterosciatic hernia is commonly the result as the herniation of the ureter into the greater sciatic foramen, usually results from the piriformis muscle weakening from increased intra-abdominal pressure due to pregnancy, constipation, surgery, trauma, as well as neuromuscular or hip diseases. Occasionally, it may be congenital [1]. Ureterosciatic hernia may occur in both children and adults, but middle-aged female adults are at greater risk due to a generally wider pelvic bone (Figure 1) [2,3].
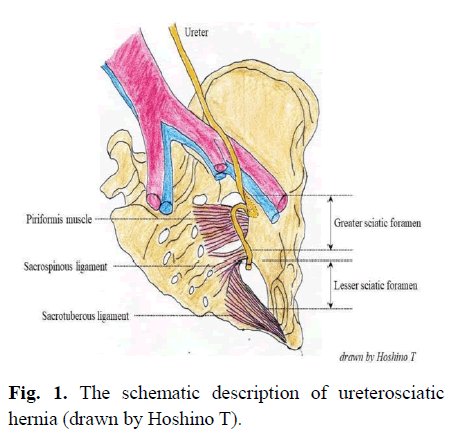
Fig. 1. The schematic description of ureterosciatic hernia (drawn by Hoshino T).
This condition may cause ureteral occlusion, and consequently lead hydronephrosis and urinary tract infection, which need urgent treatment to relieve the structural ureteral obstruction. Treatment options include surgical and conservative treatments with ureteral stenting; however, no consensus has been reached. Surgical treatment includes ureteral anastomosis, uretero-bladder neoanastomosis, and mesh reinforcement of the sciatic foramen. There have been scattered reports of laparoscopic or robot-assisted repair in recent years.
Literature Review
This case, which has been discussed in a previous paper [4], describes a 73-year-old female patient that had presented to the outpatient clinic of our hospital with complaints of left-side abdominal pain. Computed Tomography (CT) showed marked left hydronephrosis and dilation of the ureter, which herniated into the greater sciatic foramen, 4 cm from the ureteral orifice. Urgent ureteral stenting was performed and the herniated ureter was corrected. The left abdominal pain resolved after ureteral stenting. Three months later, the ureteral stent was removed and the patient experienced no recurrence. However, 4 years and 8 months later, the patient experienced left abdominal pain. CT showed an ureterosciatic hernia again. The ureteral stent was replaced, and the ureterosciatic hernia improved. The ureteral stent was removed 4 months later, but ureterosciatic hernia recurred 5 months later. This was the second recurrence; therefore, we performed a laparoscopic repair of ureterosciatic hernia. The ureteral stent was left in place until the surgery (Figure 2).
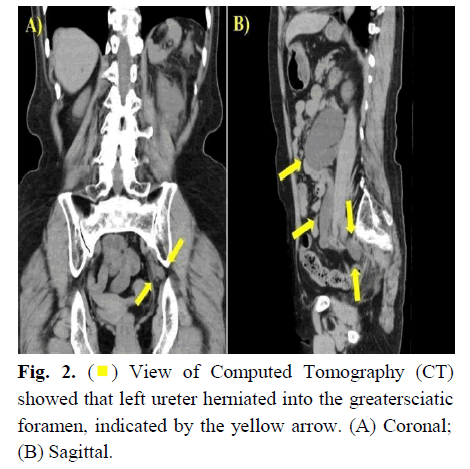
Fig. 2. ( ) View of Computed Tomography (CT) showed that left ureter herniated into the greatersciatic foramen, indicated by the yellow arrow. (A) Coronal; (B) Sagittal.
) View of Computed Tomography (CT) showed that left ureter herniated into the greatersciatic foramen, indicated by the yellow arrow. (A) Coronal; (B) Sagittal.
Methodology
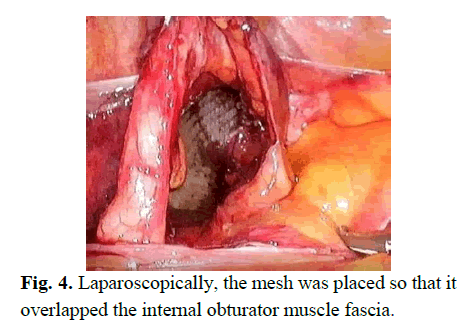
Surgery was performed under general anaesthesia in the supine position with the head lowered by approximately 20 °. A 12-mm camera port was placed above the umbilicus using the open method. The surgeon stood on the right side of the patient, with the scopist and assistant on the left side. The sigmoid colon was dissected from the peritoneum. The left ureter is identified at the crossing point of common iliac artery. The peritoneum just above the ureter was incised and the ureter was dissected circumferentially and secured using tape. The secured ureter was dissected peripherally. Simultaneously, the ventral dissection around the ureter was minimized and the dorsal, lateral, and medial sides were mainly dissected to facilitate subsequent suturing of the peritoneum of the incision (Figure 3).
Fig. 3. The ports placement of laparoscopic surgery. Note:  Camera port (12 mm);
Camera port (12 mm);  Surge On left hand port (12 mm);
Surge On left hand port (12 mm);  Surgeon right hand port (12 mm);
Surgeon right hand port (12 mm);  Assistant port (5 mm)
Assistant port (5 mm)
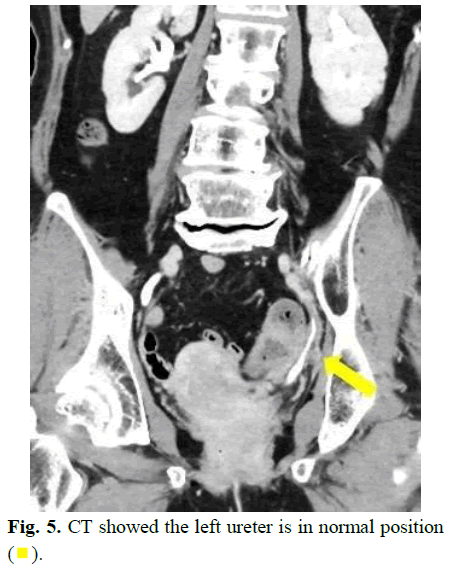
The medial umbilical ligament, uterine artery, and obturator vein were identified, and the internal obturator muscle was identified with the dissection of the ureter. The internal obturator muscle fascia was peeled off to facilitate implantation of the distal end of the mesh. No apparent hernia foramen was observed during the operation. However, the outer side of the ureter, slightly cephalad to the internal obturator muscle, was easily peeled off and sufficient space was formed. Therefore, we speculated that the ureter had fallen in this vicinity. The fixed part of the mesh was determined and the mesh size was selected to fit the peeled area. Bird® Ventralite® ST was trimmed into a 7 × 3.5 cm rectangle. The mesh was inserted into the body cavity through a 12-mm port and placed such that the distal end overlapped the internal obturator muscle fascia (Figure 4).
Fig. 4. Laparoscopically, the mesh was placed so that it overlapped the internal obturator muscle fascia.
The incision was closed, with continuous sutures using 3-0 V-LocTM (Medtronic) to allow the ureter to enter the retroperitoneal cavity. A 5-mm J-VAC® (ETHICON) was inserted through the 5-mm assistant port on the left side, placed so that the tip was near the peritoneal suture, and the procedure was terminated. The operative time was 2 h 30 min, insufflation time was 2 h 4 min, and blood loss was minimal. The patient was discharged from the hospital on postoperative Day 7 without complications. A month post-surgery, the ureteral stent was removed. Two months postoperatively, there was no left hydronephrosis. The patient had no recurrence of pain at one year postoperatively (Figure 5).
Fig. 5. CT showed the left ureter is in normal position ( ).
).
Results and Discussion
Traditionally, most of ureterosciatic hernias are repaired by an open surgery including a manual reduction of the hernia and resection with re-implantation of ureter in some cases. With the development of laparoscopic technology, laparoscopic surgery for ureterosciatic hernia is a more minimally invasive procedure, and the magnified field of view and good spatial exposure make the quality of surgery more excellent. Recently, robot assisted laparoscopic surgical technology is well suited to facilitating and enabling major advanced pelvic surgery including urological, gynecological and digestive surgical procedures. However, ureterosciatic hernia does not have an established treatment. Conservative treatment includes the placement of a ureteral stent to correct the fitted ureter. There have been a few cases of recurrence [5-8]. Gee et al. reported the first laparoscopic repair, in which a mesh was placed near the pisiform muscle [5]. Tsuzaka et al. reported laparoscopic suturing of the connective tissue around the sciatic foramen and closure of the hernia foramen without using a mesh [9]. Singh et al. reported robot- assisted ureterobladder neoanastomosis [10], and Regelman et al. reported robot-assisted suturing of the connective tissue around the foramen sciaticum [11].
Kakimoto et al. reviewed 30 cases of ureteral foramen sciaticum hernias reported in 1999. As initial treatment, 21, 6, 1, and 2 patients underwent stenting, surgical treatment, manual reshaping, and follow-up, respectively [12]. Seven of the 21 patients who had undergone stent implantation reported additional surgical treatment. Several cases of recurrence have been reported with conservative treatment, whereas no cases of recurrence have been reported with surgical treatment. Furthermore, surgical treatment is preferred for curative purposes. Laparoscopic surgery is less invasive than open surgery and allows for early postoperative recovery. However, difficult dissection due to inflammation or other factors may necessitate conversion to laparotomy or uretero- bladder neoanastomosis [13].
In our patient, pain improved after ureteral stenting and ureteral stent was removed thereafter. However, the disease recurred twice. As this patient had no major underlying disease and was relatively young, ureteral stent replacement was not desirable; therefore, we decided to treat the patient surgically. Regarding preoperative ureteral stenting, preoperative ureteral stenting hinders the visualization of the hernia pit. In the present case, no apparent hernia pores were observed; however, a space that appeared to be a hernia pore was observed. Anatomically, placing a mesh in front of the internal obturator muscle may be sufficient to prevent herniation of the ureteral foramen sciaticum.
With regard to hernia defect, it was handled by multiple surgical methods previously. Closure of the defect by ligation and suturing of the sac or patching across the prosthetic mesh is performed to prevent recurrence of the hernia. In some cases, no repair is performed in asymptomatic patients [5]. However, there is no literature that provides reliable long-term results among these types of repairs. Preoperative placement of a ureteral stent may prevent urinary tract infections and facilitate a safe surgical approach. Since there is no established surgical technique for this disease, further review of cases is warranted.
Conclusion
We discussed the ureterosciatic hernia utilizing our experienced successful treatment by laparoscopic surgery which had been recurred repeatedly after conservative treatment. Conservative treatment has limited efficacy, and surgery should be considered in some cases. Ureterosciatic hernia in children is an exceedingly rare condition where the ureter herniates into the sciatic foramen. When conservative treatments fail or in cases of recurrent herniation, laparoscopic surgical intervention may be considered. The laparoscopic approach involves making small incisions, utilizing a camera for visualization, and repairing the hernia with minimal tissue disruption. This technique offers potential advantages in reduced postoperative pain, shorter hospital stays, and quicker recovery compared to traditional open surgery. However, the decision for laparoscopic treatment should be carefully evaluated based on the individual case, considering factors such as the child’s overall health and the specific characteristics of the hernia.
References
- Seifarth FG, Kundu N, Magnuson DK. Congenital sciatic hernia. Pediatr Surg Int. 2014; 30(5):541-543.
[Crossref] [Google Scholar] [PubMed]
- Smith CW, Undre S, Salter V, et al. An unusual case of a ureteric hernia into the sciatic foramen causing urinary sepsis: Successfully treated laparoscopically. Ann R Coll Surg Engl. 2007; 89(7):W10-12.
[Crossref] [Google Scholar] [PubMed]
- Bohnert WW. Ureteral sciatic hernias: Case report of an infant with bilateral ureteral herniation into the sciatic foramina. J Urol. 1971; 106(1):142-143.
- Hoshino T, Sejima T, Iwamoto H, et al. The rare urological entity of ureterosciatic hernia: A case report of successful treatment after repeated recurrence. Urol Case Rep. 2023; 11(51):102562.
[Crossref] [Google Scholar] [PubMed]
- Gee J, Munson JL, Smith JJ. Laparoscopic repair of ureterosciatic hernia. Urology. 1999 Oct;54(4):730-7333.
[Crossref] [Google Scholar] [PubMed]
- Kato T, Komiya A, Ikeda R, et al. minimally invasive endourological techniques may provide a novel method for relieving urinary obstruction due to ureterosciatic herniation. Case Rep Nephrol Dial. 2014; 5(1):13-9.
[Crossref] [Google Scholar] [PubMed]
- Yanagi K, Kan A, Sejima T, et al. Treatment of ureterosciatic hernia with a ureteral stent. Case Rep Nephrol Dial. 2015; 5(1):83-6. .
[Crossref] [Google Scholar] [PubMed]
- Whyburn JJ, Alizadeh A. Acute renal failure caused by bilateral ureteral herniation through the sciatic foramen. Urology. 2013; 81(6):e38-9.
[Crossref] [Google Scholar] [PubMed]
- Tsuzaka Y, Saisu K, Tsuru N, et al. Laparoscopic repair of a ureteric sciatic hernia: Report of a case. Case Rep Urol. 2014; 787528.
[Crossref] [Google Scholar] [PubMed]
- Singh I, Patel B, Hemal AK. Robotic repair of a rare case of symptomatic "Ureterosciatic Hernia". Indian J Urol. 2013; 29(2):136-138.
[Crossref] [Google Scholar] [PubMed]
- Regelman M, Raman JD. Robotic assisted laparoscopic repair of a symptomatic ureterosciatic hernia. Can J Urol. 2016; 23(2):8237-8239.
[Google Scholar] [PubMed]
- Kakimoto K, Hikone M, Nagai K, et al. Urosepsis secondary to ureterosciatic hernia corrected with ureteral stent placement: A case report and literature review. Int J Emerg Med. 2021; 14(1):67.
[Crossref] [Google Scholar] [PubMed]
- Touloupidis S, Kalaitzis C, Schneider A, et al. Ureterosciatic hernia with compression of the sciatic nerve. Int Urol Nephrol. 2006; 38(3-4):457-458.
[Crossref] [Google Scholar] [PubMed]
Author Info
Takahiro Hoshino1, Takehiro Sejima1*, Hideto Iwamoto1 and Youji Fukumoto22Department of Gastrointestinal Surgery, Matsue City Hospital, Matsue, Japan
Received: 15-Nov-2023, Manuscript No. PUCR-23-119801; , Pre QC No. PUCR-23-119801; Editor assigned: 20-Nov-2023, Pre QC No. PUCR-23-119801; Reviewed: 04-Dec-2023, QC No. PUCR-23-119801; Revised: 11-Dec-2023, Manuscript No. PUCR-23-119801; Published: 18-Dec-2023, DOI: 10.14534/j-pucr.20222675614
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.