Case Report - (2023) Volume 10, Issue 4
Penoscrotal hypospadias with intact foreskin: A rare exception to the two-zipper hypothesis presentation
Devon Thomas1, Seyed Behzad Jazayeri1, Preeya Mistry2, Erica Mercer2 and Andrew Stec2*Abstract
The precise mechanisms of urethral development are not fully understood, but several hypotheses have been proposed to explain the formation of the urethra. One hypothesis is based on the concept of inductive signaling, which suggests that the surrounding tissues play a crucial role in developing the urethral epithelium. According to this theory, signals from the mesoderm and intermediate mesoderm, as well as growth factors from the surrounding tissues, work together to induce the differentiation and growth of the urethral epithelium. The two-zipper theory is a model that explains the underlying mechanisms of hypospadias formation.Keywords
Urethral epithelium, Mesoderm, hypospadias, Reconstruction, Pediatric urology, urethral development, urethraIntroduction
According to this theory, hypospadias is caused by a combination of inadequate mesenchymal growth and inappropriate epithelial growth. In this theory, the urethral flat plate is formed as the first unzipped layer followed by a sequential and testosterone dependent interlacing zipping effect in an antegrade fashion leading to complete formation of urethra and closure of the prepuce, which is hypothesized to depend on the formation of urethra. One exception to this hypothesis is the megameatus variant with intact prepuce. In this paper, we present an extremely rare variant of hypospadias with penoscrotal junction opening of the urethra with intact prepuce formation and partially formed distal urethra and open glans [1].
Case Presentation
A 5-week-old white male was referred to our pediatric urology clinic by his primary pediatrician for concerns of hypospadias as well as possible duplicated urethra. He was delivered at 34 weeks gestation due to intrauterine growth restriction and required an 11 day stay in the NICU at birth. On initial urologic consultation, it was noted that he had circumferential preputial skin distally with phimosis and a large open area on the mid-penile shaft that lacked ventral skin. There was an opening noted underneath his prepuce that appeared to be an intact distal glandular urethra and in addition it was clear that he had proximal penoscrotal hypospadias. His parents stated that his entire urinary stream came from the proximal urethral opening, and they had never seen urine come through his phimotic foreskin or distal opening. Based on in-office exam there was no evidence of duplicated urethra. This variant of hypospadias had never been observed in our practice and we have not been able to find any other reports of this variant in the literature (Figures 1 and 2) [2].
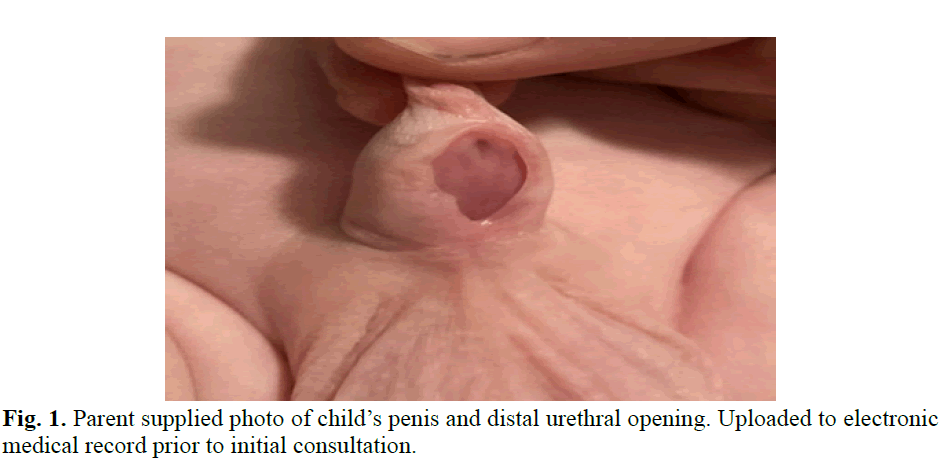
Fig. 1. Parent supplied photo of child’s penis and distal urethral opening. Uploaded to electronic medical record prior to initial consultation.
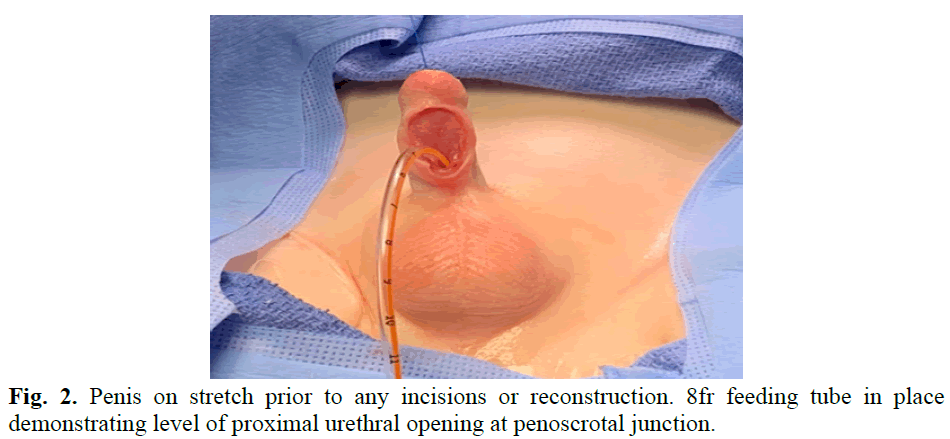
Fig. 2. Penis on stretch prior to any incisions or reconstruction. 8fr feeding tube in place demonstrating level of proximal urethral opening at penoscrotal junction.
Our patient underwent a one stage hypospadias repair at 10 months of age with primary tubularization of the urethra and closure of the ventral penile shaft skin. Intra-operatively further examination was performed prior to beginning the repair and he was again noted to have a phimotic distal prepuce, completely intact circumferentially, with hypospadias in the penoscrotal location. The urethral plate was abundant and wide and was visible from the penoscrotal junction all the way up to the bottom part of the glans. It had the appearance as if the ventral surface of the phallus had been unzipped. An 8fr feeding tube was able to be passed through the proximal urethral opening as well as through the distal urethra, which had intact urothelium without corpus spongiosum tissue. It was also noted under anesthesia that the patient had a mild, 20-degree, ventral chordee which was not appreciated on in-office exam. This was corrected with Nesbit plication sutures prior to proceeding with urethral reconstruction. The urethra and urethral plate were well mobilized, the intact distal urethra was opened, and the entire penile urethra was tubularized in a two-layer urethroplasty using 7-0 vicryl suture and then covered with a dartos flap for additional coverage and to ensure non-overlapping suture lines. Glans wings were also created and mobilized to cover the distal portion of the urethra. Tension-free reconstruction and good cosmesis were achieved by the conclusion of the procedure (Figures 3 and 4) [3].
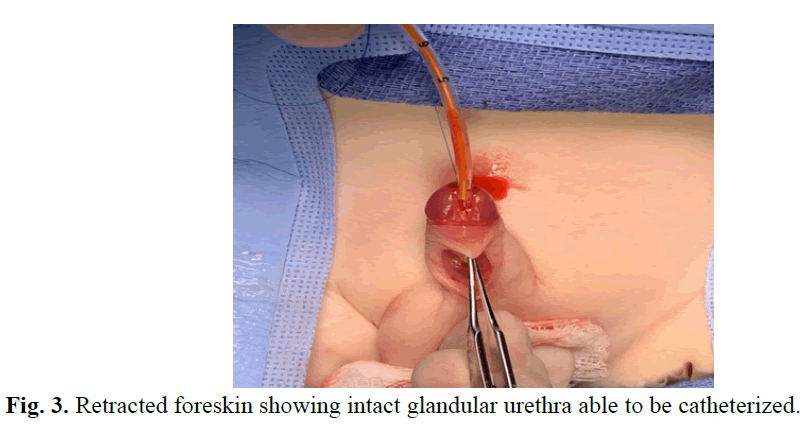
Fig. 3. Retracted foreskin showing intact glandular urethra able to be catheterized.
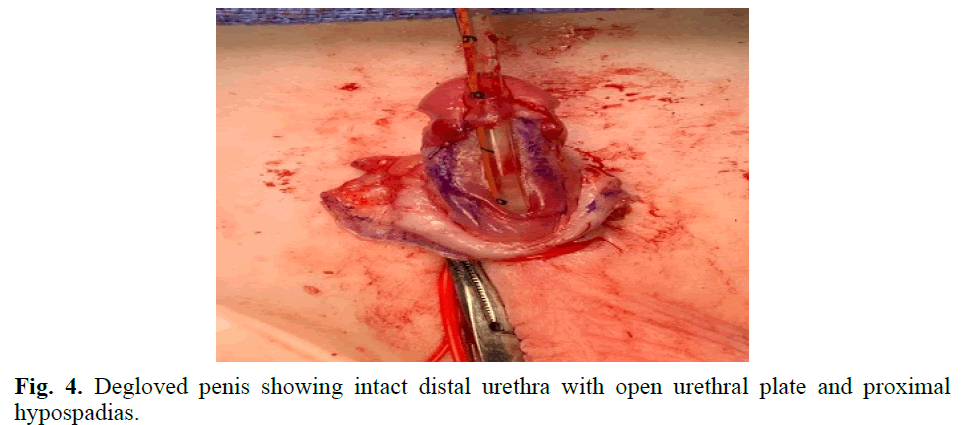
Fig. 4. Degloved penis showing intact distal urethra with open urethral plate and proximal hypospadias.
Results and Discussion
Hypospadias affects approximately 1 in 250 new-born males and is the second most common anomaly of the genitalia. The majority of hypospadias cases are due to unknown causes but are considered to be related to genetic susceptibility and environmental exposure in utero either before or during urethral development. A small number of patients have associated genetic syndromes or abnormalities in androgen metabolism such as congenital adrenal hyperplasia, 5-a-reductase deficiency, and androgen insensitivity.
Hypospadias remains a confusing presentation to many non-GU providers. There is a wide range of presentations and can be seen as a distal megameatus with variations as severe as atypical genitalia that prompt workup for a disorder of sex development. The three hallmark features that have been thought to accompany nearly all hypospadias cases are an ectopic urethral meatus, chordee, and a dorsally hooded foreskin/ventral foreskin deficiency. Multiple rare variants have been described in the literature to date, but none have noted the rarities seen in our case [4-6].
There are few variants that exist in a very small subset of patients such as duplicated urethra and intact prepuce megameatus. One rare urethral pathology that most closely resembles our case presentation on physical exam is that of congenital anterior urethrocutaneous fistula. Though this condition is often thought to be a complication of circumcision there have been many cases reported with the condition being present since birth. There are two presentations of congenital urethrocutaneous fistula; the first is isolated fistula which is associated with normal foreskin, and absence of chordee or hypospadias (Figure 5).
Conclusion
These patients have intact distal urethra and spongiosum. The second type of congenital anterior urethrocutaneous fistula is often seen to have hypospadias features such as foreskin deficiencies and chordee with or without an intact distal urethra. Patients with this urethral variant are often reconstructed in a very similar manner to our patient with long term success rates up to 90% with a single surgical procedure4. Although our workup and surgical approach are not novel, this case is important due to its interesting anatomic variant that does not follow the expected embryological pathways.
References
- Partin AW, Dmochowski RR, Kavousi LR, et al. Embryology of the Genitourinary Tract. Campbell-Walsh-Wein Urology. 2020; 1(1):305-312.
[Google Scholar] [PubMed]
- Baskin L. What Is Hypospadias? .Clinical Pediatrics. 2017; 56(5):409-418.
- Hassan A, Kotb M, Shehata S. Congenital anterior urethrocutaneous fistula: A case report and review of literature. Urol Case Rep. 2019.
[Crossref] [Google Scholar] [PubMed]
- Bhatnagar A, Upadhyaya VD, Kumar B. Congenital urethrocutaneous fistula: Case report with review of literature. Indian J Plast Surg. 2012; 45(3):563-565.
[Crossref] [Google Scholar] [PubMed]
- Tennenbaum SY, Palmer LS. Congenital urethrocutaneous fistulas. Urology. 1994; 43(1):98-9.
[Crossref] [Google Scholar] [PubMed]
- Nakane A, Hayashi Y, Kojima Y, et al. Congenital urethrocutaneous fistula. Int J Urol. 2000; 7(1):343–4.
[Crossref] [Google Scholar] [PubMed]
Author Info
Devon Thomas1, Seyed Behzad Jazayeri1, Preeya Mistry2, Erica Mercer2 and Andrew Stec2*2Division of Urology, Nemours Children’s Health, Jacksonville, USA
Received: 21-Jul-2023, Manuscript No. PUCR-23- 107707; , Pre QC No. PUCR-23- 107707 (PQ); Editor assigned: 28-Jul-2023, Pre QC No. PUCR-23- 107707 (PQ); Reviewed: 11-Aug-2023, QC No. PUCR-23- 107707; Revised: 21-Aug-2023, Manuscript No. PUCR-23- 107707 (R); Published: 29-Sep-2023, DOI: 10.14534/j-pucr.20222675598
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
