Case Report - (2022) Volume 9, Issue 4
Surgical management of a Type IIA-1 complete urethral duplication: A case report
Ranger Kile1*, Ruomei Wu2 and Matthew Timberlake2Abstract
Urethral duplication is a rare congenital anomaly of the genitourinary tract with several possible anatomic variations and clinical presentations. Owing to its rarity and variability, best practices for diagnosis and intervention have yet to be defined. Management must therefore be individualized, focusing on preserving voiding and continence, preventing troublesome sequalae such as infection, and achieving normal cosmesis. Here we describe an asymptomatic 5-month-old boy with Effmann type IIA-1 complete urethral duplication confirmed by cystourethroscopy and retrograde urethrogram. The family was counseled on options of observation versus surgical excision, and opted for operative intervention. Open cystotomy was performed, with identification of the accessory urethra with retrograde instillation of methylene blue. The proximal portion of the urethra was then excised with multilayer closure. To avoid sphincteric injury, the prostatic/bulbar segments were not excised. The distal accessory penile urethra was then excised and a circumcision was performed. The patient experienced no postoperative complications. Our case illustrates a safe and effective surgical technique for localizing and excising a type IIA-1 urethral duplication while minimizing risk of injury to the sphincteric mechanism and neurovascular structures.
Keywords
Accessory urethra, double urethra, congenital anomaly, malformation, urethral excision
Introduction
Urethral Duplication (UD) is a rare congenital anomaly with varying clinical presentations. Anatomic variations identified include the following: a blind-ending accessory urethra or completely duplicated urethras arising from either a single or duplicated bladder system, as depicted in Figure 1 [1]. UD presents primarily in males and can manifest as urethral discharge, urinary incontinence, infection, double urinary streams, outflow obstruction, or even penile curvature. However, most patients have an asymptomatic presentation [1-5]. Owing to its rarity and anatomic variability, formal guidelines for diagnosis and management have yet to be established [3-5,6,7]. Interventions must therefore be individualized according to the anatomical and clinical presentation of each patient, as well as family preference after thorough discussion of risks, benefits, and alternatives [3,5]. Here we report a case of successful conservative surgical treatment of an Effmann type IIA-1 complete urethral duplication in a 5-month-old male.
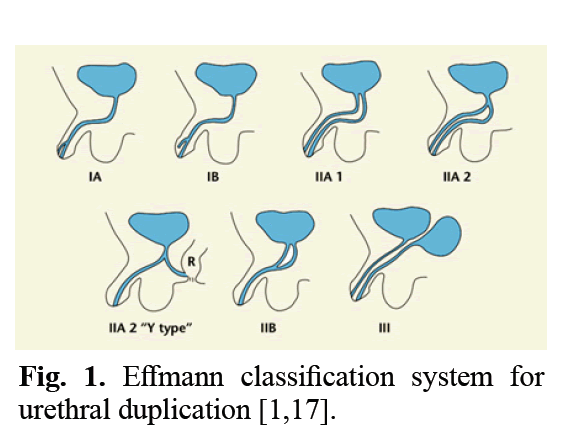
Figure 1: Effmann classification system for urethral duplication [1,17].
Case Presentation
A 3-day-old male was found during routine neonatal circumcision to have a dorsal penile anomaly prompting concern by the pediatrician for an epispadias variant. Pediatric urology evaluation was obtained. Physical exam demonstrated a groove along the dorsum of the glans and a pit near the dorsal coronal margin. He was asymptomatic with no history of unexplained fevers, urinary tract infections, or voiding dysfunction. Initial fluoroscopic Voiding Cystourethrography (VCUG) demonstrated no evidence of bladder or bladder neck anomaly, reflux, or UD. At 5 months of age, the child underwent Cystourethrography with retrograde urethrogram, seen in Figure 2. This demonstrated the presence of an accessory dorsal urethra entering the bladder, confirming Effmann type IIA-1 complete urethral duplication. The family was counseled on options of observation versus surgical excision, with detailed education regarding potential risks of each approach. After thoughtful consideration, they preferred to proceed with operative intervention. The patient underwent surgical intervention at 15 months of age. Cystourethroscopy was performed via the normal ventral urethra. The location of the accessory urethra in the bladder could not be visualized endoscopically. Open cystotomy was then performed. Methylene blue was instilled in retrograde fashion through an angiocatheter directed up the accessory urethral meatus. This allowed identification of the insertion of the accessory urethra within the bladder. The accessory urethra entered the bladder approximately 2 centimeters anterior and superior to the bladder neck. The accessory outlet was then excised with a multilayer bladder closure. To avoid sphincteric injury and preserve continence, the prostatic/bulbar segments were left intact. The penis was carefully degloved and the distal accessory urethra was excised to the level of the mid-shaft. The proximal penile accessory urethra did not produce any dorsal penile curvature and was left intact to scar down. Circumcision was then completed with an overall aesthetic outcome. The patient experienced no intraoperative or postoperative complications and was discharged on postoperative day 1. At his two-month and then one-year follow-up, the patient was doing well with normal voiding and no infections.
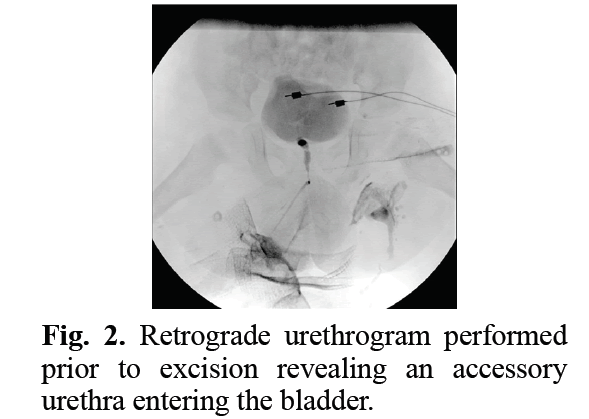
Figure 2: Retrograde urethrogram performed prior to excision revealing an accessory urethra entering the bladder.
Results and Discussion
Urethral duplication is a rare congenital anomaly primarily observed in males and often associated with other genitourinary or gastrointestinal anomalies [2,3,5,8]. Currently, the most widely accepted classification system is that of Effmann, et al. which focuses on anatomical appearance rather than embryologic origin [1,7]. Summarized in Table 1 and Figure 1, the Effmann classification defines three types of UD. Effmann type I, an incomplete urethral duplication, is a blind-ending accessory urethra and consists of two subtypes. In type IA (distal) there is an accessory urethra that opens on the dorsal or ventral penile surface that has no communication with the urethra or bladder. In type IB (proximal) an accessory urethra originates from the normal urethra but ends blindly in periurethral tissue. Type II, or complete urethral duplication, is similarly composed of two subtypes. Type IIA consists of a completely duplicated meatus and is further divided into subtypes IIA-1 and IIA-2. Type IIA-1 demonstrates two noncommunicating urethras each arising independently from the bladder, while type IIA-2 demonstrates a Y-type urethral duplication arising from the bladder, maintaining independent channels distally. Type IIB represents duplicated urethras arising from either the bladder or the posterior urethra that ultimately join into a single channel and form a single meatus. Lastly, type III describes urethral duplication arising from partial or complete caudal duplication [1]. Radiologic investigation is necessary for diagnosing UD and identifying the functional urethra. Most commonly, this is the ventrally located urethra, as was illustrated by our patient [5,9,10]. Initial radiologic evaluation is most often done with a VCUG and retrograde urethrography [4,11,12]. Other less common radiologic evaluations include Contrast-Enhanced Voiding Urosonography (ceVUS) and Magnetic Resonance Imaging (MRI) [12,13]. Still, diagnosing UD can be challenging due to its anatomic variation and often asymptomatic presentation [1,3,7,9,14]. Proper diagnosis and clinical severity are the most critical aspects in determining the correct treatment of UD. Higher-grade types often require multiple complex surgeries while milder presentations can often be observed [3,4,9]. Treatment should thus be tailored to individual concerns from the patient and family as well as the severity of presentation [1,2,5,10,14]. It has been largely suggested that only symptomatic patients require surgical intervention. Current literature indicates most patients that present with UD undergo surgical repair, however, the possibility of underdiagnosis in asymptomatic patients should be considered [1-4,9]. Development of new surgical techniques have also led to the increased repair of milder presentations, due to concerns of poor cosmesis and/or function as the patients develop [15]. Choosing not to repair UD may result in urinary stasis leading to chronic infection and inflammation [3]. In our case of type IIA-1 UD, the family felt that the risk for potential complications of infection, pelvic abscess, and incontinence outweighed the risks of a conservative surgical excision. Following thorough discussion with the family regarding options of complete excision versus partial excision, they elected for partial excision (proximal and distal obliteration), allowing the prostatic and proximal penile accessory urethra to remain in vivo. We extensively reviewed potential downsides of a partial excision, including recanalization or the possibility of a malignancy of the intact segment of the accessory urethra later in life. In our case, the family preferred these risks to those of a more invasive surgical excision. Many other techniques for repair have been described, including obliteration of the accessory channel via injection of a sclerosing agent, urethrourethrotomy, complete surgical excision of the accessory urethra, and complete urethral reconstruction [6,7,14,16]. A modified excision of the accessory urethra is currently the safest and most effective intervention, as damage to the sphincteric mechanism and neurovascular bundles can be avoided [6,14,17]. Like the methods demonstrated by Alanee, et al. and Yanai, et al. in which they used modified techniques from epispadias and hypospadias repair, respectively, we opted for the utilization of surgical methods familiar to pediatric urologists [13,15].
| Type | Description |
|---|---|
| Type I | Incomplete urethral duplication |
| Type IA (distal) | An accessory urethra opens on the dorsal or ventral penile surface that has no communication with the urethra or bladder |
| Type IB (proximal) | An accessory urethra originates from the normal urethra but ends blindly in periurethral tissue |
| Type II | Complete urethral duplication |
| Type IIA1 | Two noncommunicating urethras arising independently from the bladder |
| Type IIA2 | a.Single urethra arising from the bladder with a second originating from the first, maintaining an independent channel distally |
| b.Y-type - Single urethra arising from the bladder splits, with one communicating with the glans and the other the rectum or perineum | |
| Type IIB | Two urethras arising from either the bladder or the posterior urethra ultimately joining into a single channel forming a single meatus |
| Type III | Urethral duplication arising from partial or complete caudal duplication |
Table 1: Effmann classification of urethral duplication [1].
Conclusion
Our approach to intervention successfully identified and obliterated the accessory urethra without presenting any risk to the primary urethra, sphincteric mechanism, or neurovascular bundles. Our case illustrates a safe, familiar, and effective technique for localizing and excising an Effmann type IIA-1 urethral duplication while preserving the primary urethra, sphincteric mechanism, and neurovascular structures. As there is limited literature on the subject, we hope the contribution of our experience will provide guidance to other surgeons caring for children with this rare anomaly.
References
- Effmann EL, Lebowitz RL, Colodny AH. Duplication of the urethra. Radiology. 1976; 119(1):179-185.
- Arena S, Arena C, Scuderi MG, et al. Urethral duplication in males: Our experience in ten cases. Pediatr Surg Int. 2007; 23(8):789-794.
[Cross Ref] [Google Scholar] [Pubmed]
- Guglielmetti LC, Delcont M, Walker J, et al. Urethral duplication—epidemiology, diagnosis, and treatment in a case series of 19 patients. J Pediatr Urol. 2020; 16(3):385-e1.
[Cross Ref] [Google Scholar] [Pubmed]
- Suoub M, Saleem MM, Sawaqed F. Complete urethral duplication: Case report and literature review. Res Rep Urol. 2020; 12-15.
[Cross Ref] [Google Scholar] [Pubmed]
- Wani SA, Munianjana NB, Jadhav V, et al. Urethral duplication in children: Experience of twenty cases. J Indian Assoc Pediatr Surg. 2019; 24(4):275.
[Cross Ref] [Google Scholar] [Pubmed]
- AbouZeid AA, Safoury HS, Mohammad SA, et al. The double urethra: Revisiting the surgical classification. Ther Adv Urol. 2015; 7(2):76-84.
[Cross Ref] [Google Scholar] [Pubmed]
- Podesta ML, Medel R, Castera R, et al . Urethral duplication in children: Surgical treatment and results. J Urol. 1998; 160(5):1830-1833.
[Cross Ref] [Google Scholar] [Pubmed]
- Ramareddy RS, Alladi A, Siddappa OS. Urethral duplication: Experience of four cases. J Indian Assoc Pediatr Surg. 2012; 17(3):111.
[Cross Ref] [Google Scholar] [Pubmed]
- Lopes RI, Giron AM, Mello MF, et al. Urethral duplication type influences on the complications rate and number of surgical procedures. Int Braz J Urol. 2017 Nov; 43:1144-1151.
[Cross Ref] [Google Scholar] [Pubmed]
- Onofre LS, Gomes AL, Leao JQ, et al. Urethral duplication-a wide spectrum of anomalies. J Pediatr Urol. 2013; 9(6):1064-1071.
[Cross Ref] [Google Scholar] [Pubmed]
- Bhadury S, Parashari UC, Singh R, et al. MRI in congenital duplication of urethra. Indian. J Radiol Imaging. 2009; 19(3):232-234.
[Cross Ref] [Google Scholar] [Pubmed]
- Patel H, Watterson C, Chow JS. Case of urethral duplication seen by voiding urosonography. Clin Imaging. 2018; 49:106-10.
[Cross Ref] [Google Scholar] [Pubmed]
- Alanee S, Gupta P, Gleich P, et al. Complete urethral duplication: Description of surgical approach mimicking distal epispadias repair. J Pediatr Urol. 2012; 8(4):343-7.
[Cross Ref] [Google Scholar] [Pubmed]
- Middleton AW, Melzer RB. Duplicated urethra: An anomaly best repaired. Urology. 1992; 39(6):538-42.
[Cross Ref] [Google Scholar] [Pubmed]
- Yanai T, Kawakami H, Nango Y, et al. Minimally invasive repair of hypospadiac urethral duplication. Pediatr Surg Int. 2011; 27(1):115-8.
[Cross Ref] [Google Scholar] [Pubmed]
- Salle JL, Sibai H, Rosenstein D, et al. Urethral duplication in the male: Review of 16 cases. J Urol. 2000; 163(6):1936-40.
[Cross Ref] [Google Scholar] [Pubmed]
- Baid M, Dutta A. Urethral duplication in a 15-year-old: Case report with review of the literature. Rev Urol. 2014; 16(3):149.
[Google Scholar] [Pubmed]
Author Info
Ranger Kile1*, Ruomei Wu2 and Matthew Timberlake22Department of Urology, Texas Tech University Health Sciences Center, Lubbock, TX, USA
Received: 15-Jul-2022, Manuscript No. PUCR-22-70275; , Pre QC No. PUCR-22-70275; Editor assigned: 20-Jul-2022, Pre QC No. PUCR-22-70275; Reviewed: 29-Jul-2022, QC No. PUCR-22-70275; Revised: 09-Aug-2022, Manuscript No. PUCR-22-70275; Published: 16-Aug-2022, DOI: 10.14534/j-pucr.20222675583
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
