Case Report - (2021) Volume 8, Issue 5
Indirect inguinal hernia containing the uterus and ovaries in premature female infants about a case
Balla Keita, Mamadou Madiou Barry*, Alpha Tour�, Mohamed Lamine Sadou Sacko, Thierno Saidou Barry and Daniel Agbo-panzoAbstract
Introduction: Inguinal hernias containing the uterus, adnexa, and fallopian tubes in preterm infants is a clinical entity very rarely reported in the literature. The case is reported to alert the exiguous frequency of this clinical entity and to remind that surgical repair can be simple and classical.
Case report: A girl of 54 days of age was received in outpatient clinic for a firm and painless left non-expansive inguinal swelling born prematurely. Surgery through an open inguinal approach was scheduled and performed after two weeks. The sac contained the uterus, adnexa, and tubes. Contralateral exploration found a residual sac which was also repaired. The postoperative course was simple.
Discussion: Embryologically there is no reliable explanation why the uterus and its adnexa should be herniated in the girl. The majority of authors agree that the elongation of the suspensory ligaments of the ovaries and the non-fusion of the mullerian ducts are factors that increase the mobility of these ducts and are therefore a possibility of deviation. Despite the rarity of this clinical presentation, dissociation of the sac from its sac can be easy and a classical cure by ligation and upper resection of the sac is a possibility.
Conclusion: We would like to point out, in addition to the small frequency of this clinical entity, that the surgical cure is classic like any hernia in children. We recommend a contralateral exploration.
Keywords
Inguinal hernia, uterus, herniorrhaphy
Introduction
The most common congenital anomaly of infancy is indirect inguinal hernia, with incidence rates of 0.8% to 4.4% affecting more boys than girls and more premature than full-term infants. In girls the sac most often contains the ovaries in about 20% of cases, sometimes associating the fallopian tube [1,2]. However, only a few cases contain the adnexa and the uterus in the hernia sac. We report the case because of its rare presentation in preterm infants in order to draw the attention of pediatric surgeons for proper management.
Case Report
An infant at 54 days of age weighing 3 kg 400 gm, first in order of gesture, born preterm at 32 weeks by voice and by non-consanguineous parents who was referred to pediatric surgery as an outpatient for left inguinal swelling. The swelling was non-reducible, painless, and firm in consistency (Fig 1). There was no external genitalia abnormality. Elective surgery was proposed through an inguinal approach (Fig 2). On exploration, the uterus, ovaries and both fallopian tubes were found in the left hernia sac (Fig 3). Careful liberation without difficulty and reintegration of the organs into the pelvic cavity; ligation of the high sac. A contralateral open herniorrhaphy revealed a small sac which was also repaired (Fig 4). No preoperative radiological examination was performed. The postoperative period was uneventful and the patient was allowed to return home the same day after a calm awakening and satisfactory postoperative observation.
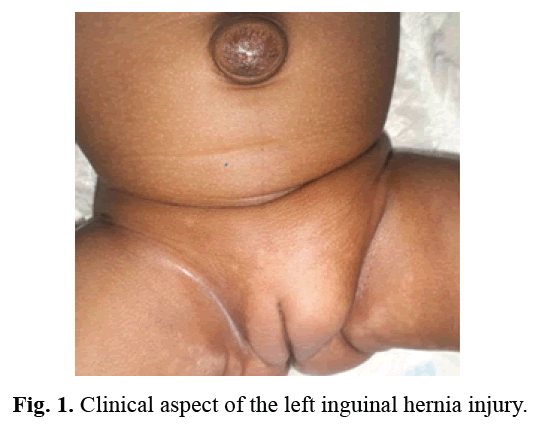
Figure 1: Clinical aspect of the left inguinal hernia injury.
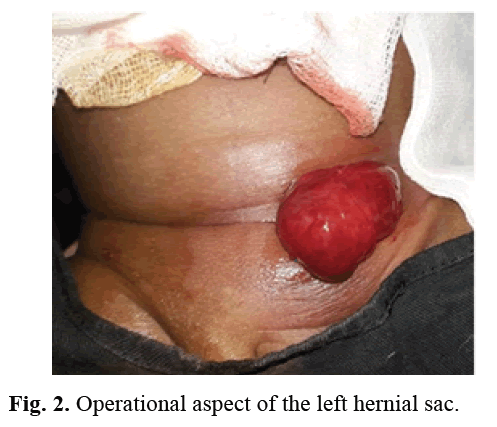
Figure 2: Operational aspect of the left hernial sac.
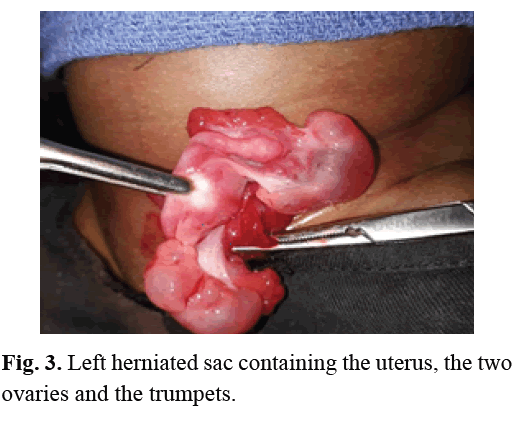
Figure 3: Left herniated sac containing the uterus, the two ovaries and the trumpets.
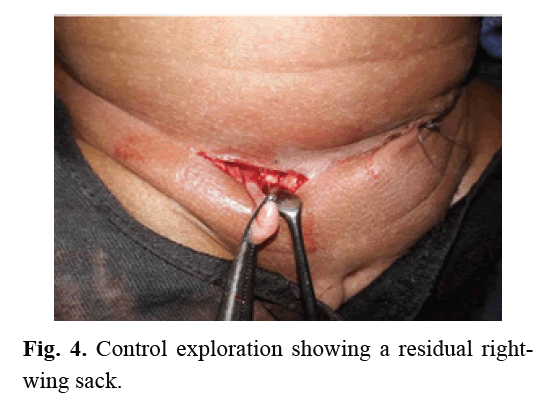
Figure 4: Control exploration showing a residual rightwing sack.
Discussion
Inguinal hernias are the most common causes of inguinal masses in infants with incidence rates of 0.8%-4.4% [1]. The process occurs as an evagination of the parietal peritoneum around the sixth month after conception. The female counterpart of the process vaginalis is relatively at 8 months of gestation, if the permeability persists it is called Nuck canal. In the literature hernias containing the ovary with or without the tube is not uncommon in female infants. However, an inguinal hernia containing the uterus is extremely rare. A few rare cases are reported in the literature. Some previous reports have presented isolated cases of incarceration of the uterus and ovary in the hernia sac in subjects of different ages [1-3]. In our case the uterus, both ovaries and fallopian tubes were in the sac in a premature baby. To our knowledge, only E.A. Marshall had reported a similar case [4]. Embryologically there is no reliable explanation why the uterus should herniate in a girl unless there is an anatomical abnormality of the ligaments that suspend the uterus [2]. A few rare cases associated with Mayer-Rakitansky-Kuster-Hauser syndrome have been described in elderly subjects. Thomson hypothesized that failure to fuse the mullerian ducts would result in excessive mobility of the ovary and that failure to fuse the uterine horns would increase the risk of herniation of the uterus, ovary and fallopian tube. On the other hand, Fowler hypothesized that elongated ovarian suspensory ligaments were the primary cause or secondary effect of a hernia [5,6].
Inguinal hernias are more frequent on the right side occurring in about 60% of cases; 30% on the left side and 10% bilateral. In our case it was on the left side. In the literature there are some rare cases describing the diagnosis and cure of inguinal hernias containing the uterus, fallopian tubes and ovary in women, the majority of these reports recommends ultrasound as the modality of choice for diagnosis, although the techniques and timing of repair have varied, although it has been shown that ultrasound systematically identifies the presence of the uterus in the hernia sac [2]. In the literature, many authors advocate rapid surgical management of indirect hernias in the girl child. However, some surgeons have delayed the cure for up to 4 weeks, while others were forced by the emerging situation [4-7]. This was the case in our case. In our context the delay in surgery did not affect the viability of the herniated organs in the absence of signs of strangulation despite the evidence that inguinal hernias containing the ovary are at greater risk of incarceration compared to those containing only the bowel or omentum about 43%. The same aspect has been reported by [4]. Our surgical approach was to separate the uterus, fallopian tubes and ovaries from the hernia sac, return them to the pelvic cavity through the inguinal canal, and then we performed a high ligation of the hernia sac. However, other surgeons, Okada and Marshall, have advocated an additional repair of the deep inguinal ring to avoid recurrence. We opted for contralateral exploration and found a residual sac on the right. The same procedure has been used by other surgeons [7,8]. We recommend contralateral exploration to avoid the infant having to undergo another surgery, especially when the location is on the left in a premature subject. Many surgeons choose to explore the contralateral inguinal region at the time of the open procedure based on data from the literature that concomitant inguinal hernias occurred in 25% of females and another study reported that the contralateral patent rate in defects of the processus vaginalis in female preterm infants was as high as 76.9% [8-10]. A previous report states that the cure of indirect inguinal hernia can be performed laparoscopically, but this requires skill and mastery of the technique, even in the hands of highly experienced surgeons, the conversion by an open inguinal approach is 10% [9].
Conclusion
In presenting this case, we have attempted to highlight the exiguous prevalence of this rare clinical entity. In the absence of signs of strangulation, the approach that, surgical correction on the basis of emergency or emergent is appropriate.
References
- Artas H, Gurbuzer N. Inguinal hernia containing both ovaries and the uterus in an infant. J Ultrasound Med. 2012; 31: 1138-1139.
- Muthiyal S, Kini V, Kounsal A. Rarity in conspicuity-ultrasound diagnosis of sliding left inguinal hernia through canal of Nuck with uterus, fallopian tubes and ovaries. Eur J Rad Open. 2016; 3: 35-37.
- Takezoe T, Sato K, Watanabe T. A female infant with an inguinal hernia containing the uterus and bilateral ovaries. J Ped Surg Case Reports. 2015; 3: 46-47.
- Marshall EA, Hao SB, Rodeberg DA. Incarcerated uterus and bilateral ovaries in a premature female infant inguinal hernia. J Ped Surg Case Reports. 2020; 52:101330.
- Thomson GR. Complete congenital absence of the vagina associated with bilateral herniae of uterus, tubes and ovaries. Br J Surg. 1948; 36: 99-100.
- Fowler CL. Sliding indirect hernia containing both ovaries. J Pediatr Surg. 2005; 40: e13-14.
- Okada T, Sasaki S, Honda S. Irreducible indirect inguinal hernia containing uterus, ovaries, and fallopian tubes. Hernia. 2012; 16: 471-473.
- Karadeniz Cerit K, Ergelen R, Colak E. Inguinal hernia containing uterus, fallopian tube, and ovary in a premature newborn. Case Rep Pediatr. 2015.
- Kara T, Seckin E, Durmaz MS. Indirect inguinal hernia containing uterus, fallopian tube, and ovary in a term infant. Ped Urol Case Rep. 2018; 5: 89-93.
- Hamidi H, Rahimi M. Infantile presentation of the canal of nuck hernia containing uterus and ovary: A case report. Radiol Case Rep. 2020; 15: 2557-2559.
Author Info
Balla Keita, Mamadou Madiou Barry*, Alpha Tour�, Mohamed Lamine Sadou Sacko, Thierno Saidou Barry and Daniel Agbo-panzoReceived: 27-Jul-2021 Accepted: 10-Aug-2021 Published: 17-Aug-2021, DOI: 10.14534/j-pucr.2021267559
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
